Flexible Benefits
Healthcare reform, search form.
Benefits Buzz

Group Health Plans: Owners, Non-Employees & Domestic Partners

Ask the Expert
Stay Connected
- Health Insurance
- Medicare Plans
- Life Insurance
- Health Savings Accounts
- Ancillary/Voluntary Plans
- Wrap Document Services
- Flexible Spending Accounts
- Federal COBRA
- Health Reimbursement Arrangements
- Compliance dashboard
- Non-Discrimination Testing
- Premium Only Plans
- Commuter Benefits
Individuals
- Press Releases
Affiliations
Headquarters, field office.
5050 Quorum Drive, Suite 700, Dallas, TX 75254 Phone: 866-472-0883 Fax: 214-292-8832
Individuals & Employers
Sales & Service: 866-472-5351
General Agency: Sales & Quotes: 888-353-9178 Service: 866-472-5352
Flex Plans: Sales & Service: 888-345-7990
Login/Register
© Flexible Benefit Service LLC. All Rights Reserved. Site Map | Privacy Policy | Terms of Use

| You might be using an unsupported or outdated browser. To get the best possible experience please use the latest version of Chrome, Firefox, Safari, or Microsoft Edge to view this website. |
- Health Insurance
What Is Group Health Insurance & How Does it Work?

Updated: Feb 27, 2024, 6:19am

Nearly 50% of insured Americans receive health insurance coverage through group plans provided by employers, according to 2019 Census data. However, many of them may not have thought much about how exactly this group health insurance works.
Group health insurance provides many benefits, but when your insurance plan is tied directly to your employment, you risk a sudden loss of health coverage should your job situation change. In 2017, 22% of uninsured Americans reported losing their health insurance due to job loss or change in employment status.
Whether you recently started a new job and want to learn more about how your new group coverage works, you already have group coverage and want to know more about it, or you just lost or quit your job and worry you’ve lost health insurance coverage, this guide can help you understand the ins and outs of group health insurance.
What Is Group Health Insurance and How Does It Work?
Group health insurance—sometimes called employer-based coverage—is a type of health insurance plan offered by an employer of a member organization. Members of a group health insurance plan usually receive coverage at a lower cost because the risk to the insurer is distributed across multiple members.
Under the Affordable Care Act (ACA), businesses with 50 or more full-time employees must provide health insurance to full-time employees and dependents under the age of 26 or pay a fee. Insurers are also required to provide group coverage to organizations with as few as two employees. Some states allow self-employed individuals to qualify for group coverage plans as well.
Group health insurance plans are selected and purchased by companies or organizations and then offered to employees. In most states, a group insurance plan is required to have a 70% participation rate, though some states’ minimum rate is higher or lower.
Benefits of Group Health Insurance Plans
Group health insurance policies have a number of advantages and benefits over individual plans. Many employers provide supplemental health plans, which include dental coverage, vision coverage and pharmacy coverage, either separately or as a bundle.
The main benefit group plans offer is lower premiums. According to 2018 research conducted by eHealth, a private online marketplace for health insurance, the average premium cost per individual in a group health insurance plan was $409 a month compared to $440 for an individual plan. In the same study, small group health plans had an average deductible of $3,140 a year compared to $4,578 for individual plans.
Additionally, family members and dependents can be added to group plans at an additional cost to members, which can assist families with sole providers or whose alternative or individual health plan options carry significantly higher prices.
Group health insurance plans provide numerous tax benefits to both the employer and employee. The money employers pay towards monthly premiums is tax-deductible, and employees’ premium payments can be made pre-tax, which may reduce their total taxable income.
Some smaller businesses may also qualify for the small business health care tax credit . The small business health care tax credit benefits an employer with fewer than 25 full-time employees who pays average wages of less than $50,000 a year, offers a qualified health plan through the Small Business Health Options Program (SHOP) Marketplace and pays at least 50% of the cost of health care coverage for each employee (but not for family or dependents).
Who Can Sign Up for Group Health Insurance?
To be eligible for group health insurance, an employee must be on payroll and the employer must pay payroll taxes. Individuals usually not eligible for group coverage include independent contractors, retirees and seasonal or temporary employees. Employees who are on unpaid leave are often ineligible for group coverage until they return to work.
Generally, group health insurance coverage must also be offered to an employee’s spouse and dependent children until age 26, though employers may choose to expand the age definition for child dependents. Employers may also opt to extend health benefits to unmarried partners of the same or opposite sex, and that coverage must mirror the coverage extended to spouses on the same plan.
How to Enroll in Group Health Insurance
To enroll in a group health care plan provided by your employer, ask about the deadline for enrollment once hired. If you miss this deadline, you might have to wait until the annual open enrollment period to join. Some employers may have waiting periods of up to 90 days before new employee health insurance kicks in. You won’t have to pay premiums during this time, but you won’t have access to any health care coverage, either.
Some group health insurance plans offer different tiers of coverage or supplemental coverage like dental, vision and/or pharmacy. During open enrollment periods, you can make decisions about these insurance choices your employer provides, as well as add or remove any dependents. If a major life event like marriage, the birth of a child or a spouse’s loss of employment changes your circumstances, you may be able to enroll these new dependents in your group health insurance plan outside the open enrollment period.
Where to Find Group Health Insurance Plans
The most common way to get group health insurance coverage is through an employer. If your employer doesn’t offer health insurance due to the small size of the company or if you’re unsatisfied with your employer’s coverage options, look into coverage through a membership organization. If you belong to a membership organization offering a group health plan, such as AARP, the National Association of Female Executives, the Writer’s Guild of America or the Freelancers Union, you may be able to get health insurance coverage through your membership.
Be wary of plans offered by some membership organizations, as many offer a “health services discount” plan, which may save you money on prescriptions but isn’t a true health insurance plan.
Featured Small Business Health Insurance Partners
UnitedHealthcare
1.3 million

On UnitedHealthcare's Website
Blue Cross Blue Shield
1.7 million

On Healthcare.com's Website
1.2 million
Group Health Insurance for the Self-Employed
Approximately 25.7 million small businesses in 2017 were considered “nonemployers,” or businesses with no paid employees, according to a 2020 report from the U.S. Small Business Administration Office of Advocacy. If your business doesn’t have any employees, you’re considered a small group of one.
Even though you’re self-employed, you may be able to buy group health insurance for your company in certain states. Check with your state’s insurance department to determine whether your state allows group policies to be sold to groups of one.
What to Do If You Lose Your Group Health Benefits
If you lose your job, you may also lose your employer-sponsored group health insurance. You and your dependents may be able to keep this coverage through what’s called continuation coverage.
In 1985, Congress passed the Consolidated Omnibus Budget Reconciliation Act (COBRA), which allows employees who lose their jobs to buy group health coverage for themselves or for their families for a limited amount of time. Under COBRA, the same group insurance plan with the same benefits must be made available to the terminated worker; however, the former employee must pay the full cost—including whatever the employer has previously covered—of the plan.
Continuation coverage is often much more expensive than an individual health insurance plan, so consider the price, benefits and network of providers carefully before making the choice to keep your coverage through continuation coverage temporarily instead of moving to an individual plan.
Featured Health Insurance Partners
Offers plans in all 50 states and Washington, D.C.
About 1.2 million
About 1.7 million
About 1.5 million

- Health Insurance Coverage of the Total Population . KFF. Accessed 9/17/2021.
- 27+ Affordable Care Act Statistics and facts . Policy Advice. Accessed 9/17/2021.
- What is the Average Cost of Small Business Health Insurance? eHealth. Accessed 9/17/2021.
- 2020 Small Business Profile . U.S. Small Business Administration Office of Advocacy. Accessed 9/17/2021.
- Group Health Plan . HealthCare.gov. Accessed 9/17/2021.
- What constitutes a group for health insurance? People Keep. Accessed 9/17/2021.
- Health Insurance During Employment . Legal Aid at Work. Accessed 9/17/2021.
- Offer SHOP health insurance . HealthCare.gov. Accessed 9/17/2021.
- Employer Health Insurance Versus Individual Plans . Medical Mutual. Accessed 9/17/2021.
- Small Business Health Care Tax Credit and the SHOP Marketplace . Internal Revenue Service. Accessed 9/17/2021.
- Eligible Employees and Dependents . Health Coverage Guide by Small Business Majority. Accessed 9/17/2021.
- Health Insurance Guide . California Department of Insurance. Accessed 9/17/2021.
- Available Through Professional and Trade Organizations . The Hartford. Accessed 9/17/2021.
- The Best Way to Buy Group Health Insurance for Self-Employed Workers . HealthMarkets. Accessed 9/17/2021.
- Health Insurance After Employment: COBRA . Legal Aid at Work. Accessed 9/17/2021.
- Best Affordable Health Insurance
- Best Dental Insurance
- Best Disability Insurance
- Best Health Insurance
- Best Health Insurance For College Students
- Best Health Insurance for Retirees
- Best Health Insurance for Young Adults
- Best Mental Health Insurance
- Best Short-Term Health Insurance
- Best Small Business Health Insurance
- Best Vision Insurance
- Compare Health Insurance Quotes
- Cost Of Health Insurance
- Cost Of Obamacare
- Does Insurance Cover Ambulance Rides?
- How Long Can You Stay On Your Parent’s Health Insurance?
- How Much Does An Urgent Care Visit Cost?
- How Much Does It Cost To Have A Baby?
- How To Get Health Insurance?
- How To Get Health Insurance Without A Job?
- What Happens If You Don’t Have Health Insurance?
- What Is Private Health Insurance?

Navigating Health Insurance As A Self-Employed Worker: 3 Things You Need To Know
No-Deductible Health Insurance: What Is It And How Does It Work?
Top Benefits Of A Health Insurance Plan In 2024

What’s The Difference Between A Deductible vs. Out-of-Pocket Maximum?

Best Health Insurance Companies Of July 2024

Best Short-Term Health Insurance Companies Of 2024
Chauncey grew up on a farm in rural northern California. At 18 he ran away and saw the world with a backpack and a credit card, discovering that the true value of any point or mile is the experience it facilitates. He remains most at home on a tractor, but has learned that opportunity is where he finds it and discomfort is more interesting than complacency.
Alena is a professional writer, editor and manager with a lifelong passion for helping others live well. Before coming to Forbes Health, Alena worked as a digital media consultant for both B2B and B2C health-focused companies for several years, building content strategies and leaning into the world of e-commerce. She is also a newly minted functional medicine certified health coach.
Mitigate misclassification risk with coverage up to USD 500,000 | Learn more
- Log In Sign Up Book a Demo
How to provide health insurance for non-employees
Things to consider around health benefits for non-employees.

PUBLISHED ON
May 12, 2022
One of the top benefits a company can offer its employees is health insurance coverage . This gives workers access to a group policy, which often allows them to secure more affordable and comprehensive coverage than they could on their own.
But what if you want to provide health insurance for non-employees, such as contractors?
While your options may be limited, there are ways to provide health insurance to non-employees. Through careful consideration of the details, you can provide contractors with a high-level benefit that will strengthen your relationship.
Before we go any further, remember this: you’re under no legal obligation to offer health insurance to individual contractors. This is a decision your company can make at its own discretion.
The best path forward is to offer contractors the same health insurance as your employees. This makes it easier to manage payroll and benefits , thus reducing the risk of error and saving you time.
If you opt to offer contract medical insurance, there are four points to keep in mind:
1. Employers can offer the same group plan
As noted above, you can offer contractors the same group plan as your part and full-time employees. You don’t have to select a different plan for contractors to access.
2. The contractor may need to declare it as taxable income
Urge your contractors to discuss the tax implications of receiving health insurance from your company. They may need to declare any employer contribution as taxable income.
3. Employers don’t have to pay any portion of the premium
There’s no requirement for employers to pay any portion of the premiums for contractors. You can do this if you want, but it’s not an obligation. That holds true even if you pay some or all of the premium for your employees.
4. Contractors may be able to deduct the premium paid
Contractors may be able to deduct any premiums paid from their income. This can help reduce the impact of the cost at tax time.
Want to see the Oyster platform in action? Book a demo and we promise to show you all the features that’ll make your People Ops team go whoa .
Is health insurance for non-employees a good idea.
There’s no right or wrong answer to this question, as the situation varies from company to company and contractor to contractor. If you’re on the fence, here are some benefits of offering health insurance coverage to “1099 employees.”
- Health insurance can help retain contractors. One of the primary disadvantages of working as a contractor is a lack of access to benefits such as medical coverage. You can help contractors by giving them access to your group policy.
- It can save you money. The more people you have on your group policy — especially if you add younger, healthier contractors — the better chance there is of reducing premiums for your entire team.
- It can help you qualify: For instance, if you’re the only employee at your company, you may need to add contractors to qualify for group health insurance.
Questions to ask and answer
As you inch closer to making a final decision, answering these questions can help you proceed with confidence:
- How many contractors do you work with?
- Do you generally maintain long-term relationships with your contractors?
- Can you afford to pay a portion of contractor health insurance premiums?
- Do you know if some or all of your contractors are interested in buying coverage through your group plan?
- Does it make sense to search for a different health insurance provider before allowing contractors to join?
Answering these questions provides insight into your situation so that you can make a more informed decision.
Oyster is here to help
Deciding for or against health insurance for non-employees is easier said than done. For that reason, you want to gather as much information and professional guidance as possible. And that’s where Oyster can help.
Oyster Health makes it simple and affordable to offer health insurance to team members in more than 180 countries. You’re not limited to offering coverage to contractors and employees in your home country.
By working directly with various health insurance carriers, Oyster can provide you with multiple quotes to help you make the right decision for your team and your company financials.
About Oyster
Oyster is a global employment platform designed to enable visionary HR leaders to find, hire, pay, manage, develop and take care of a thriving global workforce. It lets growing companies give valued international team members the experience they deserve, without the usual headaches and expense.
Oyster enables hiring anywhere in the world with reliable, compliant payroll, and great local benefits and perks. Try Oyster out with a free demo!
.webp)
Table of Contents
Related terms, additional resources.

Do employers have to offer health insurance?
Are you required to provide healthcare to your team?

Health insurance for foreign nationals
How to provide health insurance to foreign nationals.

What’s the difference between public and private health insurance?
Understanding different types of insurance for employees.

How much is health insurance for 1099 workers?
Must-knows about insurance for independent contractors.

What countries offer free health care?
Find out which countries have universal health care.

What are the most common employee benefits?
Find out what the 10 most common employee benefits are.
.webp)
How to add 1099 and global contractors to your company’s benefits plan
Learn about the benefits your company can offer contractors.
.webp)
What is an employer-sponsored health plan?
Learn how it supports employee well-being
Get A Demo of Oyster
A call from one of our Oyster experts
A full overview of Oyster's tools and features
The best available price to fit your company needs
- Updated Terms of Use
- New Privacy Policy
- Your Privacy Choices
- Closed Captioning Policy
Quotes displayed in real-time or delayed by at least 15 minutes. Market data provided by Factset . Powered and implemented by FactSet Digital Solutions . Legal Statement .
This material may not be published, broadcast, rewritten, or redistributed. ©2024 FOX News Network, LLC. All rights reserved. FAQ - New Privacy Policy
How to Get Group Health Insurance Without an Employer
Just because you are self employed or don’t work for a company that offers group health insurance, that doesn’t mean you can’t get it.
Depending on the state you live in, there are ways to get group health insurance through associations and membership organizations.
Unlike individual health insurance plans that include an underwriting process that requires a health exam and have a high turn down right, with group health insurance, the chances of getting coverage declined are minimal and the coverage includes all the major benefits. Group coverage also tends to have much smaller deductibles than individual health care.
With group insurance “the benefits tend to be richer,” says Carrie McLean, a licensed insurance agent for eHealthInsurance.com . “You might have a smaller deductible and unlimited doctor visits.”
Group Coverage for One or Two
Although not widespread, according to eHealthInsurance.com some states, including Massachusetts, Washington, New York, Florida and Colorado allow groups of one to be eligible for group health insurance.
California and New Jersey allow two-person businesses to buy group insurance for one person, if one employee has group insurance from another source, like a spouse’s employer. In order to be eligible for group insurance in any state, recipients have to have documentation that they have a business.
Let’s say you run a cleaning service but the only other person on the payroll is your wife. If you live in a state that allows groups of two to get group health insurance then you would be eligible. Both of you have to actively work in the business and both must be on the payroll, according to Craig Lordigyan, an agent and managing partner at The Lordigyan Insurance Agency.
Associations and Membership Organization Coverage
If you don’t live in a state that offers group health insurance to small groups then you may be able to get the insurance by joining an association or membership organization.
In general, an association or membership organization is a group created to support the interests of people in a specific industry or trade.
For instance, The Gasoline Retailers Association provides group benefits for repair shops. So if you worked as a mechanic in a repair shop that has only two employees, that shop could offer you group coverage, says Lordigyan.
AARP also offers group health insurance. According to AARP, its Essential Premier Health Insurance Plan is similar to the health insurance plans offered by many companies to employees. Membership fees to join AARP cost $63 for five years, $43 for three years and $16 for one year.
Associations have strict criteria to be eligible to join, but if you are in a field or trade that has an association that provides group health insurance, it can be a way to get better coverage.
Before you go out and join an association, McLean advises to make sure there’s more to joining than the health insurance. According to McLean, with some membership groups, health insurance is secondary for the group. Not to mention you’ll have to pay membership fees.
“Make sure you are getting coverage the way you want to,” she says.
- Search Search Please fill out this field.
- Group Health Insurance Plan
How Group Health Insurance Works
History of group health insurance.
- Benefits of Group Health Insurance
Insurance Options for Uninsured Individuals
Example of group health insurance, the bottom line.
- Health Insurance
- Definitions A - M
Group Health Insurance: What It Is, How It Works, Benefits
Julia Kagan is a financial/consumer journalist and former senior editor, personal finance, of Investopedia.
:max_bytes(150000):strip_icc():format(webp)/Julia_Kagan_BW_web_ready-4-4e918378cc90496d84ee23642957234b.jpg)
Thomas J Catalano is a CFP and Registered Investment Adviser with the state of South Carolina, where he launched his own financial advisory firm in 2018. Thomas' experience gives him expertise in a variety of areas including investments, retirement, insurance, and financial planning.
:max_bytes(150000):strip_icc():format(webp)/P2-ThomasCatalano-d5607267f385443798ae950ece178afd.jpg)
- Health Insurance: Definition, How It Works
- What Is Group Health Insurance? CURRENT ARTICLE
- Is Health Insurance Mandatory?
- What is the Affordable Care Act?
- ACA Marketplace Plan Types
- Private Health Insurance
- Health Maintenance Organization (HMO)
- Preferred Provider Organization (PPO)
- Point-of-Service Plan
- High Deductible Health Plan (HDHP)
- Coinsurance vs. Copays
- Copay vs. Deductible
- Preexisting Condition
- Paying for Preexisting Conditions
- How Much is Health Insurance?
- Cutting Your Costs for Marketplace Health Insurance
- What Does Health Insurance Not Cover?
- How to Apply for Financial Assistance to Pay for Health Insurance
- Health Insurance Premium
- How is my Health Insurance Premium Calculated?
- Are Health Insurance Premiums Tax Deductible?
- Health Insurance Deductible
- Out-Of-Pocket Expenses Explained
- Out-of-Pocket Maximum Explained
- How to Get Health Insurance
- Best Health Insurance Companies
- Aetna vs. Cigna
- Healthcare Cost-Cutting Cautions
- Critical Illness Insurance
What Is a Group Health Insurance Plan?
Group Insurance health plans provide coverage to a group of members, usually comprised of company employees or members of an organization. Group health members usually receive insurance at a reduced cost because the insurer’s risk is spread across a group of policyholders. There are plans such as these in both the U.S. and Canada .
Key Takeaways
- Group members receive insurance at a reduced cost because the insurer’s risk is spread across a group of policyholders.
- Plans usually require at least 70% participation in the plan to be valid.
- Premiums are split between the organization and its members, and coverage may be extended to members' families and/or other dependents for an extra cost.
- Employers can enjoy favorable tax benefits for offering group health insurance to their employees.
Group health insurance plans are purchased by companies and organizations and then offered to their members or employees. Plans can only be purchased by groups, which means individuals cannot purchase coverage through these plans. Plans usually require at least 70% participation in the plan to be valid. Because of the many differences—insurers, plan types, costs, and terms and conditions—between plans, no two are ever the same.
Group plans cannot be purchased by individuals and typically require at least 70% participation by group members.
Once the organization chooses a plan, group members are given the option to accept or decline coverage. In certain areas, plans may come in tiers, where insured parties have the option of taking basic coverage or advanced insurance with add-ons. The premiums are split between the organization and its members based on the plan. Health insurance coverage may also be extended to the immediate family and/or other dependents of group members for an extra cost.
The cost of group health insurance is usually much lower than individual plans because the risk is spread across a higher number of people. Simply put, this type of insurance is cheaper and more affordable than individual plans available on the market because more people buy into the plan.
The earliest known example of group coverage for health services dates to 1798, when Congress established the U.S. Marine Hospital for Navy seamen. Participation was compulsory, with deductions coming from salaries. Other examples include the mining, lumber, and railroad industries in the late 1800s, which had a vested interest in ensuring the health of its workers.
Montgomery Ward is credited with establishing the nation’s first group health insurance policy in 1910. The policy did not reimburse workers for medical expenses, but provided cash payments to workers equal to half their wages in the event of injury or illness.
The progressive political movement of the early 1900s led to several proposals to establish compulsory national health insurance. However, these proposals failed to counter opposition from doctors, who objected to uniform fee structures; labor groups, which felt their power would be weakened; and insurance companies, which feared encroachment on their business.
Employer-sponsored group health insurance grew rapidly in the 1940s as a way for employers to get around wage controls set during World War II. In 1943, the War Labor Board introduced wage caps but did not include insurance premiums as part of the cap. As such, employers were free to offer health insurance to attract and retain workers, resulting in a tripling of health insurance coverage by the end of the war.
But this failed to address the needs of retirees and other non-working adults. Federal efforts to provide coverage to those groups led to the Social Security Amendments of 1965, which laid the foundation for Medicare and Medicaid .
Benefits of a Group Health Insurance Plan
The primary advantage of a group plan is that it spreads risk across a pool of insured individuals. This benefits the group members by keeping premiums low, and insurers can better manage risk when they have a clearer idea of who they are covering. Insurers can exert even greater control over costs through health maintenance organizations (HMOs), in which providers contract with insurers to provide care to members.
The HMO model tends to keep costs low, at the cost of restrictions on the flexibility of care afforded to individuals. Preferred provider organizations (PPOs) offer the patient a greater choice of doctors and easier access to specialists but tend to charge higher premiums than HMOs.
The percent of the U.S. population covered by employer-provided group health insurance in 2021.
The vast majority of group health insurance plans are employer-sponsored benefit plans. It is possible, however, to purchase group coverage through an association or other organizations. Examples of such plans include those offered by the American Association of Retired Persons (AARP), the Freelancers Union, and wholesale membership clubs.
Not everyone is covered by a group health insurance plan. For many decades, these uninsured people were forced to bear the cost of healthcare on their own. But that has changed.
Government-sponsored health plans are an option for those left out of employer-sponsored group health insurance. The Affordable Care Act (ACA) adopted in 2010 created a marketplace for health insurance that provides coverage to 16.3 million people as of the 2022-2023 open enrollment season.
After the passage of the ACA, taxpayers were required to show they had health insurance coverage or qualified for an exemption, or else they were required to pay a penalty described as a “shared responsibility payment.” This mandated payment was eliminated with the passage of the Tax Cuts and Jobs Act beginning in the 2019 tax year.
United Healthcare, a division of UnitedHealth Group (UHC), is one of the nation's largest health insurers. It offers a buffet of group health insurance options for all types of businesses. Include are medical plans and specialty, supplemental plans, such as dental, vision, and pharmacy.
United Healthcare offers plans under the federally-sponsored Small Business Health Options (SHOP) program, a provision of the Affordable Care Act. In most states, employers must have 50 or fewer full-time employees, although some states allow for as many as 100 employees. Businesses that pay at least 50% of the insurance premium qualify for a 50% tax credit.
Midsize businesses, with between 51 and 2,999 employees, have various options available, including bundles. Large businesses, with 3,000 or more employees, qualify as national accounts, which have more services and healthcare features, including the ability to customize plan offerings.
What Is a Group Health Plan?
Group health plans are employer- or group-sponsored plans that provide healthcare to members and their families. The most common type of group health plan is group health insurance, which is health insurance extended to members, such as employees of a company or members of an organization.
What Is a Group Health Cooperative?
A group health cooperative, also known as mutual insurance, is a health insurance plan owned by the insured members . Insurance is offered at a reduced cost, and what they collect from members is based on claims paid. The cost of care is spread out across the insured population.
How Many Employees Do You Need to Qualify for Group Health Insurance?
Many group health insurers offer plans to companies with one or more employees. The type of plans available, however, may vary according to the size of the business . For example, United Healthcare provides various plans for small businesses with 1-50 employees , midsize businesses with 51-2,999, and large employers with 3,000 or more employees.
What Are Group Health Insurance Benefits?
Group health insurance plans offer medical coverage to members of an organization or employees of a company. They may also provide supplemental health plans—such as dental, vision, and pharmacy—separately or as a bundle. Risk is spread across the insured population, which allows the insurer to charge low premiums. And members enjoy low-cost insurance, which protects them from unexpected costs arising from medical events.
How Much Does Group Health Insurance Cost?
The average group health insurance policy costs roughly $7,400 annually for an individual, with the employee paying 17% of the premium. For family coverage, the average cost was about $21,000 per year, with the employee paying 27% of the premium.
Group health insurance plans are one of the most affordable types of health insurance plans available. Because risk is spread among insured persons, premiums are considerably lower than traditional individual health insurance plans. This is possible because the insurer assumes less risk as more people participate in the plan. For employees who ordinarily would not be able to afford individual health insurance, it is an attractive benefit.
U.S. Bureau of Labor Statistics, Monthly Labor Review. “ The Development and Growth of Employer-Provided Health Insurance ,” Pages 3-4.
Marilyn J. Field and Harold T. Shapiro. “ Employment and Health Benefits: A Connection at Risk ,” Chapter 2.
National Archives. “ Medicare and Medicaid Act (1965) .”
Kaiser Family Foundation. " Health Insurance Coverage for the Total Population ."
U.S. Department of Health and Human Services. “ Biden-Harris Administration Announces Record-Breaking 16.3 Million People Signed Up for Health Care Coverage in ACA Marketplaces During 2022-2023 Open Enrollment Season .”
Internal Revenue Service. “ Individual Shared Responsibility Provision .”
United HealthCare Services. “ Small Business Health Options Program (SHOP) .”
Kaiser Family Foundation. “ 2020 Employer Health Benefits Survey .”
:max_bytes(150000):strip_icc():format(webp)/WhatIsIndemnityHealthInsurance-f5548176a8474b95a2d3b08aeb760ba3.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
Are You Covered Under A Group Health Plan?
A “Group Health Plan” (GHP) is health insurance offered by an employer, union or association to its members while they are still working. GHP coverage is based on current employment . Employers with 20 or more employees are required by law to offer current workers and their spouses who are age 65 (or older) the same GHP health benefits that are provided to younger employees.
Examples of health insurance policies that are GHPs based on current employment .
- Small or large employer-sponsored plans for its current employees,
- Self-insured plans,
- Employee organizational plans (i.e., union plans or hours banks),
- National health plans in foreign countries.
- Do not include:
- Plans that only cover self-employed individuals,
- Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage,
- Retiree coverage,
- Continued coverage based on severance pay,
- Health savings accounts,
- Veterans Affairs (VA) coverage.
If your GHP is based on current employment, you may not need Medicare Part B when you turn 65. You may get a “Special Enrollment Period” (SEP) to sign up for Part B later without a penalty after the employment or group health plan coverage ends. If you qualify, you can sign up for Part B anytime while you’re covered by an employer or union group health plan (GHP) based on current employment , or you can enroll in Medicare Part B anytime within 8 months after the employment ends or the GHP coverage ends (whichever happens first).
If you would like to learn more, there is additional information on our " Special Enrollment Period " page.
- What if I have health care protection from other plans?
- Will I get Medicare if I live outside the United States? If you are not sure how to answer these questions and you would like to learn more, read our “Medicare” booklet or talk to your personnel office.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Exploring coverage options for small businesses
Health insurance for businesses, group health insurance coverage.
- Learn more about purchasing insurance through SHOP
- See SHOP plans and prices
- How the Affordable Care Act (ACA) affects small businesses
Health reimbursement arrangements
- Qualified small employers
- Individual coverage, such as Marketplace plans
- Additional health benefits (when offered with a traditional group plan)
Health Savings Accounts and other tax-favored health plans
A type of savings account that lets you set aside money on a pre-tax basis to pay for qualified medical expenses. By using untaxed dollars in a Health Savings Account (HSA) to pay for deductibles, copayments, coinsurance, and some other expenses, you may be able to lower your overall health care costs. HSA funds generally may not be used to pay premiums.
Refer to glossary for more details.
Health Reimbursement Arrangements (HRAs) are employer-funded group health plans from which employees are reimbursed tax-free for qualified medical expenses up to a fixed dollar amount per year. Unused amounts may be rolled over to be used in subsequent years. The employer funds and owns the arrangement. Health Reimbursement Arrangements are sometimes called Health Reimbursement Accounts.
What can we help you find?
Since you asked: can an employer offer health insurance to its board’s directors.
By Maureen Gammon , Anu Gogna , Benjamin Lupin and Kathleen Rosenow | December 21, 2022
Employers often have questions on practical considerations related to healthcare, retirement and other employee benefit regulations. In this “Since you asked” feature, we discuss the provision of health insurance to board members and their dependents.
Can our company provide benefits under our group health plan to members of the company’s board of directors who are not employees? We would like to provide coverage for retention and recruiting purposes.
Possibly, but various compliance concerns need to be addressed.
Multiple Employer Welfare Arrangement considerations
Covering non-employees (whether directors, board members or owners) under a company's benefit programs is likely to raise compliance concerns (assuming the written plan eligibility rules allow non-employees to enroll in coverage). For one, it is unclear whether a Multiple Employer Welfare Arrangement (MEWA) is created when health or other welfare benefits are provided to non-employee directors.
- A MEWA is defined as an employee welfare benefit plan providing benefits to the employees of two or more employers (including one or more self-employed individuals). If the board of directors consists of members who are not current employees of the company, this would technically classify the benefit plan as a MEWA, as the non-employees would be considered self-employed individuals.
- From a federal reporting standpoint, MEWAs are generally required to file an annual report with the federal government (Form M-1); however, the plan may qualify for an exemption to filing the annual Form M-1. More specifically, a group health plan is exempt if less than 1% of participants are non-employee directors, and the plan would not be a MEWA “but for” coverage of non-employee directors. This does not mean that the arrangement is not a MEWA but only that no Form M-1 filing is required.
- MEWAs do not qualify for ERISA preemption from a state regulatory perspective, so the plan potentially would be subject to state laws specifically regulating MEWAs, including any filing and licensing requirements similar to rules imposed on insurers licensed to operate in the state. For example, California law requires self-funded MEWAs to obtain a certificate of compliance from the Department of Insurance in order to operate within the state. But under California law, the Department of Insurance ceased providing such certificates in 1995, effectively preventing the formation of any new MEWAs. In addition, since state law would likely apply, state mandated benefit rules may apply to the arrangement (e.g., requiring the plan to cover medical procedures it would not otherwise cover).
Tax considerations
Generally, the coverage for the non-employee director cannot be pre-tax under the cafeteria plan rules, although there is a special rule for certain "dual status" individuals (i.e., directors who are also employees).
- If non-employees are permitted to participate in employer-sponsored benefits, they cannot participate on a tax-favored basis in the same way as employees.
- Under the general rule, directors who are not employees of the company (“outside directors”) cannot participate in the company's cafeteria plan. This is the case whether or not the directors receive fees for their services as directors. The 2007 proposed cafeteria plan regulations expressly provide that the term “employee” does not include a “self-employed individual.” The regulations list examples of self-employed individuals: a sole proprietor, a partner in a partnership, and a director serving on a corporation's board of directors who does not otherwise provide services to the corporation as an employee. Contributions made by non-employees should be made on an after-tax basis, and contributions made by the employer should be treated as additional taxable compensation.
- The regulations also provide a special rule for certain “dual status” individuals. Under the dual status rule, an individual who is an employee and provides services to his or her employer as a director or independent contractor (e.g., an individual who is both an employee and a director of a C corporation) is eligible to participate in the employer’s cafeteria plan, although solely in his or her capacity as an employee. For example, assume one of the company's employees also serves on the company's board of directors. Her annual compensation as an employee of the company is $80,000; she also receives $5,000 in directors' fees each year. She can participate in the company's cafeteria plan in her capacity as an employee and can elect to make salary reductions from her employee compensation for benefits under the plan; however, she cannot elect to reduce her directors' fees for benefits under the plan. Note that if the company is an S corporation, the dual-status rule will not apply to any employee-directors who are also shareholders owning more than 2% of company stock at any time during a year.
- In addition, directors who are not employees cannot participate in a health reimbursement arrangement or health flexible spending account. Note: Non-employees may make contributions to health savings accounts (HSAs) as long as they are otherwise eligible (i.e., enrolled in a qualifying high-deductible health plan, have no other disqualifying coverage and cannot be claimed as a tax dependent). Any contributions made by the non-employee to an HSA should be made on an after-tax basis, which then may qualify for an above-the-line deduction on his or her individual tax return (Form 1040).
- Companies offering coverage to directors and their dependents under their group health plan need to make sure they (or their third-party administrators) have the ability to do so on an after-tax basis.
- MEWA considerations must be discussed with legal counsel, as such an arrangement may need to be registered in various states (assuming it is permitted by state law).
- A possible alternative for directors would be the company paying taxable cash (with or without a gross-up) and helping them find individual health insurance coverage.
Related Solutions

MyCompass Login Document Center

Employee Benefit Guidance & Compliance Solutions
Is offering health coverage to Non-Employees risky?
A frequent Compliance Corner question asks whether employers can include independent contractors in their health plans or other benefits. When dealing with contractors or temporary employees, many think they are not eligible for their health plans or other benefits such as COBRA or FFCRA. The answer to this question is more complicated than one might think. So, is offering health coverage to non-employees risky?
Most benefit experts advise against including independent contractors or other non-employees such as 1099 employees, non-employee directors, or leased employees on employer’s benefit plans.
Here are three (3) reasons why this may be inadvisable:
- Treating an independent contractor as an employee may undermine an employer’s assertion that the individual is not an employee. The DOL and the IRS , as well as their state counterparts, have aggressive programs to uncover worker misclassification . By offering a non-employee employee benefit, an employer’s assertion to these regulators challenging whether an individual is really an employee is weakened. Moreover, if some non-employees gain benefits while others do not, an independent contractor excluded from a plan may sue for benefits exposing an employer to potential penalties.
- Covering individuals who are not employees on the health plan may result in the creation of a multiple employer welfare arrangement or MEWA. The intent to create a MEWA is irrelevant. MEWAs have IRS reporting requirements such as Form M-1. If the plan is self-funded there may be further complications with state laws that prohibit self-insured MEWAs
- Tax issues also come into play. For example, an independent contractor is not eligible for a Section 125 plan. Employer contributions to coverage may also be taxable.
Complicating this decision is that some insurance carriers will allow independent contractors to be included in an employer’s health plan. But, compliance is the employer’s responsibility, not the insurance carrier’s.
The best answer to whether non-employees can be offered coverage is that employers who wish to evaluate or pursue covering non-employees should consult their legal and benefits advisors.
An insurance broker that is exciting? We bet you never heard that before! Believe it or not, our firm is often described as a fun and exciting place to work by our employees and carrier partners.
Over the years, our founders noticed that employees who enjoy coming to work every day, are much more productive and much better suited to represent our company. If you are going to entrust us to handle both employer and employee questions , wouldn’t you want to interact with someone who is pleasant and frequently smiles?
We truly have a unique culture at PF Compass . Our culture is shaped by our Core Values: Respect, Honesty, Commitment, and Enthusiasm. Employees at PF Compass are dedicated to these values and take many steps to prove it. Whether it’s developing knowledge by participating in educational seminars or simply reading today’s news, our staff help to continually grow the company while making us better than the competition.
if i am a 1099 employee and a certain employer says they can put me on the company medical benefit plan, what do i need to know?
December 15, 2022
I’m also interested in the answer
June 28, 2024
There is no quick and easy answer to this. It can be a complex issue, but here is all the information you need to know:
IRS Guidelines: The IRS has strict rules distinguishing between employees and independent contractors. Offering employee benefits like health insurance to 1099 workers can blur these lines and potentially reclassify the worker as an employee.
ERISA Compliance: The Employee Retirement Income Security Act (ERISA) generally governs employer-sponsored health plans and does not cover independent contractors.
Insurance Carrier Policies: Most insurance carriers do not allow 1099 contractors to be included in group health plans. They typically restrict coverage to W-2 employees to maintain compliance with state and federal regulations.
Tax Implications: If the IRS reclassifies your status from independent contractor to employee due to receiving employee benefits, it could result in back taxes, penalties, and interest for both you and the employer.
Legal Risks: Employers face legal risks if they are found to be improperly classifying workers to avoid taxes or other regulatory requirements.
July 3, 2024
Post a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- Healthcare Compliance
- Employee Education & Communication
- Benefits Admin Technology
- Account Management
- HRA Administration
- Our Purpose
- Shawn Kennedy
- Amy Gibriano
- Maribel Higgins
- Brandi Bowers
- Jared Koplik
- Valerie Harrs
- Perry Koplik
- Brian Honan
- Patty Davala
- Anthony Bruno
- Maggie Johnson
- Hilary Boff
- Mick Smoothey
- Our Culture
- Non-Profits
- HR Professionals
- Business Executives
- Our Clients
- Life Insurance
- Executive Reimbursement Plans
- Voluntary Benefits
- Time To Upgrade!
© 2015 PF Compass
Pin It on Pinterest
- StumbleUpon
SCHEDULE A PLAN REVIEW
Fill Out Our Contact Form:
All Services Healthcare Compliance Employee Education & Communication Benefits Admin Technology Account Management COBRA HRA Administration Other

- Providing world class service and value for employee benefit group plans since 1987
- 800-903-6066
How to Determine Which Employees are Eligible for Group Coverage and What it Covers

Once you’ve made the decision to offer group health insurance to your employees—either to satisfy a mandate or to boost your competitiveness in attracting talent, it’s time to start shopping. About half of the total US population is covered by group health insurance through employers , so you’re in good company. You should put together a benefits policy early on that identifies in writing who is—and is not eligible for group coverage.
While you may have control over certain eligibility decisions, proceed with caution. Your benefits policies should be designed to promote fairness. Any indication of bias or favoritism can land your company in hot water.
Which Employees are Eligible for Group Health Insurance?
An employer may choose to cover any employee on their payroll, but most choose to restrict these benefits to full-time employees that have met certain criteria like completion of a probationary period. However, if an employer offers insurance benefits to one full-time employee, they must offer the same benefits to all full-time employees.
The IRS defines a full-time employee as anyone who works an average of 30 hours or more per week. This is the definition that the Affordable Care Act will use so employers who are subject to mandated insurance coverage should align their benefits policies to this definition of a full-time employee.
Who is Not Eligible for Group Health Insurance?
Your company may employ a variety of different types of people. Not everyone fits the definition of a full-time employee, even if they meet the hourly requirement. Let’s take a look:
- Employees covered under a collective bargaining agreement may not be eligible for your group health insurance policy, particularly if their agreement provides coverage through a different plan.
- Independent contractors or freelancers that may perform work for your company are not eligible to participate in your group health plan.
- Retired or former employees are not eligible.
- Temporary employees or those who have not yet completed any probationary periods required by corporate policies may not be eligible.
- Non-employee directors or consultants are not eligible.
- Part-time employees who work less than 30 hours per week may not be eligible based on your company benefits policy.
What are Dependents and How do you Determine Eligibility?
In addition to your full-time employees, group coverage eligibility typically extends to their dependents (or immediate family members) with some caveats. A company generally must offer dependent eligibility in order to satisfy ACA . However, some smaller companies may not be able to secure low enough rates to make dependent coverage feasible. Here’s a closer look at the ins and outs:
The biological and adopted children of an eligible employee should be covered through age 26, according to the ACA. However, employers have some freedom in defining a dependent child to include stepchildren without requiring adoption or to extend the age beyond 26.
Spouse or Domestic Partners
The legal married spouse should be considered eligible in most cases. However, some states may not recognize same-sex marriages and in some cases, employers use an alternative insurance clause to deter spousal coverage.
- Domestic Partner: A long-term living arrangement with another adult without a legal marriage. Employers may choose to extend spousal eligibility to domestic partners. Policies should be specific, indicating whether this applies to same-sex domestic partners, opposite-sex domestic partners, or both.
- Alternative Coverage Clause: If a spouse or domestic partner is employed full-time and has access to reasonably-priced insurance through that employer, they may not be eligible for coverage as a spouse on your plan.
What Group Health Insurance Covers
Group health insurance is intended to cover eligible medical expenses for the employees of an organization and their dependents. Coverage limits vary by policy, but a typical group health insurance policy covers:
- Primary Care Visits
- Specialty Care Visits
- Urgent Care
- Emergency Care
- Hospitalization
- Surgical Interventions
- Diagnostics
- Preventative Care
- Maternity Care
- Mental Health Care
These policies don’t pay the full cost of these services . Instead, each policy defines a deductible, co-pay, and co-insurance amount that splits cost between the insured and the insurer.
- Deductible: The amount that the insured pays before the plan kicks in.
- Co-Pay: A fixed amount that the insured pays for designated services.
- Co-Insurance: The percentage of expenses that the insured pays after the deductible is met.
Additionally, some plans offer supplemental coverage for other services like dental care, vision, and prescriptions. If not, the employer usually secures supplemental coverage through other providers in order to offer a complete benefits package to their employees.
The Takeaway on Group Insurance Eligibility
The bottom line is that group health insurance is typically reserved for regular, full-time employees and their dependents. Any coverage extended to part-time workers or non-traditional dependents is solely at the discretion of the employer. The only requirement is that the employer must provide the same options to all employees that meet the same criteria. This coverage, which is mandated by the ACA in most cases, covers typical medical expenses for doctors visits and required care.
Written by Todd Taylor

Todd Taylor oversees most of the marketing and client administration for the agency with help of an incredible team. Todd is a seasoned benefits insurance broker with over 35 years of industry experience. As the Founder and CEO of Taylor Benefits Insurance Agency, Inc., he provides strategic consultations and high-quality support to ensure his clients’ competitive position in the market.
What Are Your Insurance Needs?
Featured Testimonial

Todd Taylor with Taylor Benefits gives our small business the kind of personal service we need. Insurance benefits are important to our employees and Todd helps us find a balance between benefits and value. Todd responds immediately to my phone calls & e-mails. He has even gotten in touch with me on a Sunday when we were in need of coverage answers immediately. We are very pleased with the hands-on service Todd and his staff provide.”
- Ken and Linda Orvick, Orvick Management Group, Inc.
Recent Post
- Murfreesboro Large Group Health Insurance Plans
- Springfield Large Group Health Insurance Plans
- Oceanside Large Group Health Insurance Plans
- Fort Collins Large Group Health Insurance Plans
- Lancaster Large Group Health Insurance Plans
- Self Employed
- Pension Plan
- Affordable Care Act
- Peoples also ask
- retirement benefits
- Employee Benefits
- Insurance claims
- good insurance companies
- Insurance claims process
- Mental Health Insurance
- Group health insurance
- Employee insurance
- employee insurance rates
- Uncategorized
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
We’re ready to help! Call today: 800-903-6066

- Core and Group Health
- Voluntary Benefits
- Consumer Driven Health Care
- Health Care Reform
- Benefits Sales Strategies
- Broker Innovation Lab
- Practice Management
- Employer-Paid
- Employee-Paid
- HR Regulation
- HR Technology
- Cost-Containment
- Employee Participation
- Defined contribution
- Advisor Sales Strategies
- Retirement Regulation
- Advisor Technology
- Retirement Trends
- Defined Benefits
- Investment Instruments
- LUMINARIES Website
- LUMINARIES Coverage
- Advisor of the Year Website
- Advisor of the Year Coverage
- Benefits Leads
- 401(k) Leads
- Career Center
- Special Reports
- BROKER EXPO
- Instant Insights
- Expert Perspectives
- Editorial Calendar
Resource Center
- Newsletters
- Podcast Center
- Asset & Logo Licensing

NOT FOR REPRINT
Page Printed from: benefitspro.com/2021/04/02/4-characteristics-of-non-group-health-insurance-enrollees/?slreturn=20240709154810
Instant Insights /
4 characteristics of non-group health insurance enrollees.
Based on what we know about existing individual-market shoppers, will the expanded ACA subsidies have a major impact on enrollment?

The Biden administration recently announced that it would be extending the special open enrollment period for health insurance coverage on the federal exchanges through August. As of early March, more than 200,000 people had taken advantage of the extended opportunity to purchase health insurance, and legislators hoped to entice even more with expanded subsidies included in the American Rescue Plan.
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing. Once you are an ALM digital member, you’ll receive:
- Critical BenefitsPRO information including cutting edge post-reform success strategies, access to educational webcasts and videos, resources from industry leaders, and informative Newsletters.
- Exclusive discounts on ALM, BenefitsPRO magazine and BenefitsPRO.com events
- Access to other award-winning ALM websites including ThinkAdvisor.com and Law.com
Already have an account? Sign In
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected] . For more information visit Asset & Logo Licensing.
Trending Stories
1 health care price transparency tools increase prices ask economists, 2 chevron overturned: how federal agencies' loss of power impacts health care and benefits, 3 experts debate: should scotus have overruled the chevron doctrine , 4 employers, take note: financial wellness benefits employees really want, 5 house republican aims to revive association health plan regulations, recommended stories, questions congressional budget office is asking about adding a benefit to medicare.
By Allison Bell | July 09, 2024
Your clients often have to decide whether adding a new benefit is worth it. Here's some of what Medicare managers consider.

Health care cost containment: filtering out the waste
By Mark Galvin | July 09, 2024
Policies implemented over the past three years empower fiduciaries to scrutinize and manage health care costs and regain control of the unsustainable cost burden weighing on employers and employees.

Health disparities exist in every state: Stark racial divide in premature deaths
By Scott Wooldridge | July 09, 2024
Massachusetts, Minnesota, and Connecticut stand out for their relatively high performance for all ethnic groups, yet these states have considerable health disparities between white and nonwhite residents, says a new report.
Infographic
Sponsored by ArmadaCare
The True Cost of Cutting Healthcare Coverage
Degrading healthcare coverage to control benefit costs can have huge ripple effects and drive-up costs in other areas. This infographic looks at the many consequences that you and your clients need to know.
Browse More Resources ›
Sponsored by Redirect Health
A Complete Broker's Guide to Self-Funded Plans
This guide provides brokers with essential insights and practical advice on implementing and managing self-funded plans to help employers save on healthcare costs while maintaining high-quality care for employees.
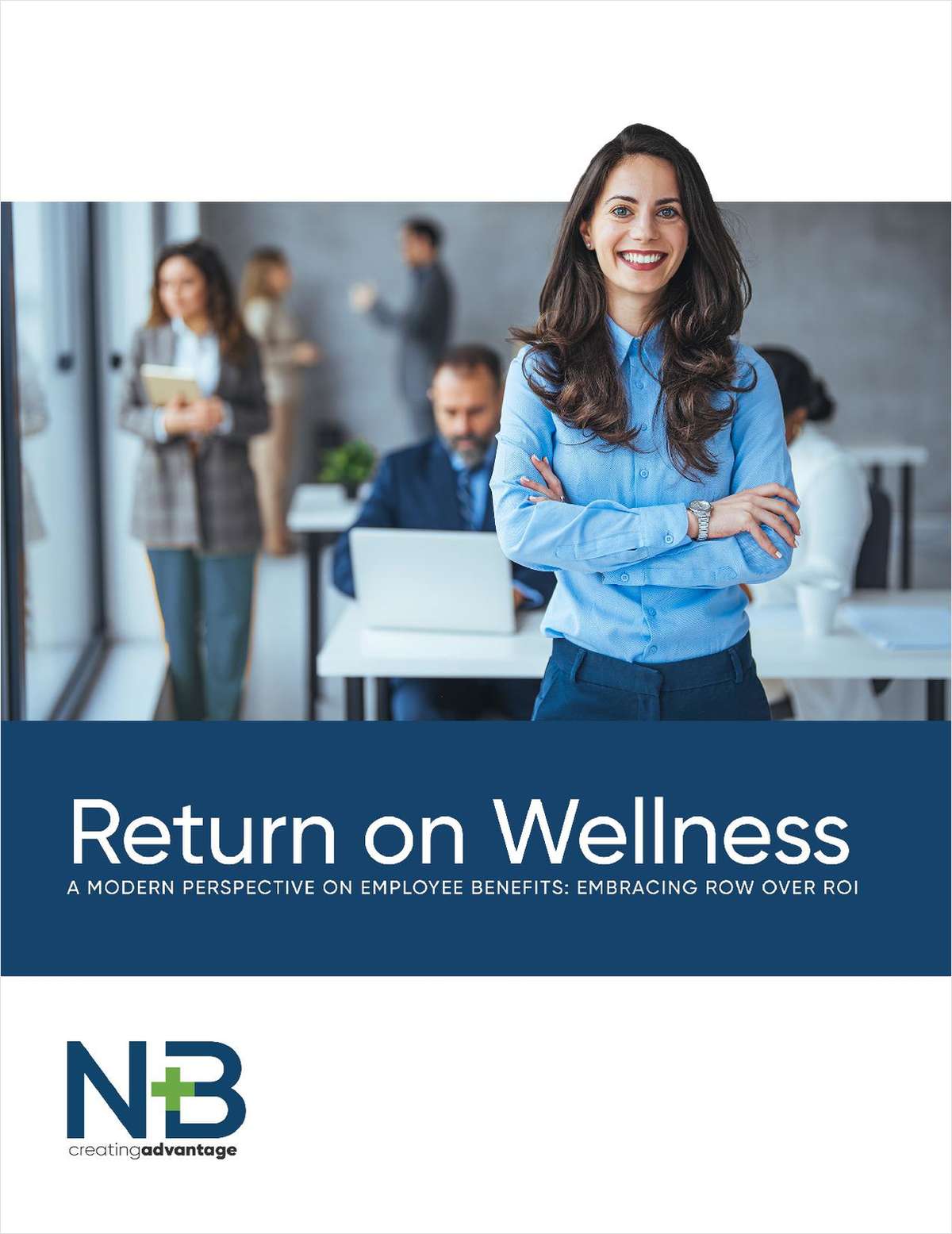
Sponsored by New Benefits
Return on Wellness: A Modern Perspective on Employee Benefits
It’s time to redefine employee benefits by shifting the focus from Return on Investment (ROI) to Return on Wellness (ROW). This guide outlines why prioritizing overall employee well-being results in a multitude of rewards, from increased productivity to reduced healthcare costs.
BenefitsPRO

Don’t miss crucial news and insights you need to navigate the shifting employee benefits industry. Join BenefitsPRO.com now!
- Unlimited access to BenefitsPRO.com - your roadmap to thriving in a disrupted environment
- Exclusive discounts on BenefitsPRO.com and ALM events
Already have an account? Sign In Now
Health Insurance for Non-Profits
There’s a reason we count more non-profits as clients than any other sector.
Health Insurance for Nonprofits: An In-depth Look at Options
Nonprofit organizations face distinct challenges when it comes to providing health benefits for their employees. Balancing the need to deliver value to their teams while maintaining financial sustainability requires innovative solutions. In this guide, we will explore the dynamic landscape of health coverage for nonprofits and highlight the advantages of Health Reimbursement Arrangements ( HRAs ), including Individual Coverage HRAs ( ICHRAs ) and Qualified Small Employer HRAs ( QSEHRAs ).
We will address the pain points nonprofits often experience, such as limited budgets and low salaries, and discuss strategies to overcome these challenges while ensuring effective stewardship of funds.
Join us as we navigate the world of health benefits for nonprofits and uncover how HRAs can be a game-changer in achieving a sustainable balance between mission-driven impact and employee well-being.
Harnessing the Power of HRAs: Supporting Employee Well-Being and Financial Sustainability in Nonprofits
According to a recent study conducted by the Urban Institute, approximately 20% of nonprofit workers in the United States lack access to employer-sponsored health insurance.
This highlights the importance of exploring innovative solutions that can help bridge this gap and support the well-being of nonprofit employees.
One such solution gaining traction is Health Reimbursement Arrangements (HRAs). HRAs offer flexibility and cost control, allowing nonprofits to allocate their limited resources efficiently while attracting and retaining top talent.
In a report published by the Society for Human Resource Management (SHRM), it was found that nonprofits with comprehensive employee benefits, including health coverage, experience higher employee satisfaction and increased productivity. This demonstrates the importance of investing in employee well-being and the positive impact it can have on nonprofit mission success.
These statistics and real-world examples underscore the significance of exploring innovative approaches to health benefits in the nonprofit sector. HRAs provide a strategic tool for nonprofits to deliver valuable health coverage, overcome budgetary constraints, and attract and retain talented individuals dedicated to advancing their organization's mission.
Join us as we delve into the world of health benefits for nonprofits, examining the advantages of HRAs and how they can help nonprofits strike a balance between financial sustainability, honoring the mission, and prioritizing employee well-being.
Nonprofits: Balancing Mission, Stewardship, and Limited Resources
As nonprofits, the core focus is undoubtedly on advancing the mission and making a positive impact. However, it's essential to acknowledge the challenges that come with limited budgets, typically low salaries, and the need to be good stewards of the funds raised or received through grants. In this section, we'll delve into these pain points and discuss strategies for nonprofits to navigate these challenges effectively.
Putting Dollars Towards the Mission, Not Overhead
Nonprofits understand the significance of directing funds towards their mission rather than overhead expenses. It's crucial to optimize the allocation of resources to ensure maximum impact. However, certain operational costs, such as employee benefits, cannot be overlooked. Health benefits, in particular, play a vital role in attracting and retaining top talent, which is essential for nonprofit success. Striking the right balance between minimizing overhead and providing competitive health benefits becomes a crucial consideration.
Being Good Stewards of Funds
Nonprofits have a responsibility to be good stewards of the funds they raise or receive through grants. Donors and grantors want to see their contributions utilized wisely and effectively. This means carefully evaluating expenditures and making strategic decisions. While it may be tempting to minimize costs across the board, it's essential to remember that investing in employee benefits, including health coverage, is an investment in the organization's long-term sustainability and success.
Navigating Nonprofit Pain Points
Limited budgets and typically low salaries present challenges for nonprofits in various ways. One of the most significant pain points is attracting and retaining talented individuals who can contribute to the organization's mission. Nonprofits often compete with for-profit entities that can offer more substantial compensation packages. As a result, finding and retaining skilled employees can be an ongoing struggle. Limited budgets can make it challenging to offer competitive benefits, further adding to the difficulty of attracting and retaining top talent.
Strategies for Success
While the pain points may seem daunting, there are strategies nonprofits can employ to overcome these challenges and thrive:
- Strategic Budgeting: Prioritize spending on areas that have the most significant impact on your mission. This may involve finding cost-effective solutions for overhead expenses while ensuring essential employee benefits, such as health coverage, are not compromised.
- Creative Compensation Packages: Consider alternative forms of compensation, such as flexible work arrangements, professional development opportunities, or unique non-monetary perks that align with your employees' values and interests. This approach can help offset the limitations of low salary budgets.
- Maximizing Health Benefit Value: Partner with benefit providers who understand the unique needs of nonprofits and offer cost-effective solutions without compromising quality. Platforms like Take Command Health can help nonprofits navigate the complexities of health benefits, providing tailored options that fit within limited budgets.
- Highlighting the Mission: Emphasize the impact and purpose of the organization's work when recruiting and engaging employees. Nonprofits often attract individuals who are passionate about making a difference, and leveraging that sense of purpose can help compensate for lower salary offerings.
By employing these strategies and prioritizing the effective utilization of resources, nonprofits can overcome the pain points associated with limited budgets, low salaries, and the need for stewardship.
By providing competitive health benefits while being mindful of costs, nonprofits can attract and retain talented individuals who share their vision and contribute to the organization's mission-driven success.
Addressing the Unique Health Benefit Challenges in Nonprofits with HRAs, ICHRAs, and QSEHRAs
Nonprofit organizations, with their distinctive mission and structural frameworks, often confront unique challenges when it comes to delivering health benefits to their employees. As these organizations strive to maximize their resources towards mission-centric activities, they are often in search of efficient, cost-effective solutions to provide robust health benefits.
Health benefits are a crucial part of the compensation package for employees, and their importance cannot be understated. However, given the unique financial and structural nuances of nonprofits, traditional group health insurance plans may not always be the most feasible or efficient way to provide these benefits.
Enter HRAs – this category of employer-funded plans allows organizations to reimburse employees for out-of-pocket medical expenses and individual health insurance premiums on a tax-advantaged basis. Within the HRA universe, two specific types – the Individual Coverage HRA ( ICHRA ) and the Qualified Small Employer HRA ( QSEHRA ) – have emerged as particularly valuable tools for nonprofits.
ICHRA and QSEHRA allow nonprofits to control costs while maintaining a high level of care for their employees. ICHRAs offer flexibility and scalability, making them a suitable choice for larger organizations, while QSEHRAs offer simplicity and cost-effectiveness, making them an attractive option for smaller nonprofits.
Exploring Health Reimbursement Arrangements (HRAs)
Health benefits are a key factor in recruiting and retaining top-tier talent in any organization, including nonprofits. But traditional health insurance plans may not always be the most cost-effective or flexible solution for these organizations. HRAs are a unique tool that could potentially transform the way nonprofits approach health benefits.
The most important thing about HRAs like QSEHRA or QSEHRA is that they allows nonprofits to reimburse employees tax-free for individual health insurance premiums and medical expenses.
This is a big deal because nonprofits can now get the same favorable tax treatment as big company group health plans but with a lot less hassle.
HRAs enable nonprofits to adopt a strategy called "defined contribution" which is much simpler than hassling with a one-size-fits all group plan and is proven to be much more efficient, affordable, and predictable.
Nonprofits can now give their employees a fixed dollar amount each month, say $200, and each employee can then shop for the plan that fits his or her needs the best.
Sally can choose a Blue Cross plan for her doctor, Roger can get Aetna to cover his prescription, and Betty can stay on her husband's group plan.
Gone are the days of comparing quotes from each insurance company or the headache of trying to get everyone what they want without breaking the budget!
And employees end up happier too.
What are HRAs?
Health Reimbursement Arrangements, or HRAs, are employer-funded health benefit plans that reimburse employees for out-of-pocket medical expenses, as well as premiums for individual health insurance policies. HRAs are not health insurance plans themselves; rather, they are a means for employers, including nonprofits, to help their employees pay for healthcare costs.
The Advantages of HRAs for Nonprofits
HRAs serve as a robust solution for nonprofits navigating the complex landscape of health benefits.
- Cost Control : One of the most significant challenges nonprofits face is budget predictability, particularly concerning healthcare costs. HRAs offer a solution to this issue by allowing nonprofits to determine how much they will contribute to each employee's HRA account each year. This fixed contribution model enables nonprofits to budget their healthcare expenses accurately and efficiently. The ability to control healthcare costs without compromising the quality of benefits offered to employees is an appealing feature of HRAs for nonprofits.
- Flexibility: Another strength of HRAs lies in their flexibility. They allow nonprofits to design a health benefit plan that aligns with their resources and the specific needs of their employees. HRAs can reimburse a broad spectrum of medical expenses, including doctor visits, prescription medications, and even health insurance premiums. This flexibility means that nonprofits can provide a health benefits package that truly supports the wellbeing of their employees.
- Tax Efficiency: Lastly, the tax advantages offered by HRAs cannot be understated. The reimbursements provided through an HRA are typically tax-deductible for the nonprofit, reducing their overall tax liability. Additionally, these reimbursements are received tax-free by the employees, thereby enhancing the value of their health benefits. This dual tax efficiency creates a win-win scenario for both the nonprofit and its employees.
Limitations of HRAs for Nonprofits
Despite their advantages, HRAs do come with certain limitations:
- Complexity: HRAs come with rules and regulations that can seem daunting. The complexity of understanding, implementing, and managing these plans may appear as a hurdle to some nonprofits. However, with Take Command, this challenge is effectively mitigated. Our platform simplifies the setup, administration, and compliance of HRAs, making these health benefits solutions accessible and manageable for nonprofits, regardless of their size or resources.
- Limited Scope: While HRAs provide a substantial contribution to health coverage, they might not cover all health expenses. Employees may need to complement their HRA with an individual health insurance policy. With Take Command’s personalized support and user-friendly platform make it easier for employees to navigate the health insurance marketplace and find a plan that complements their HRA benefits.
Leveraging HRAs' cost-efficiency, flexibility, and tax benefits, nonprofits can build a robust health benefits strategy. With Take Command’s expert guidance, nonprofits can effectively manage HRAs, aligning their health benefits with their mission, ensuring employee wellness, and financial sustainability.
Which HRA is right for you?
Case study: qsehra success in nonprofits - new britain roots.
New Britain ROOTS, a small nonprofit based in Connecticut, promotes food security and empowered eating choices through local advocacy and education initiatives. With a small team and limited funding, the organization faced a significant challenge: providing affordable health benefits for their staff.
Executive Director, Joey Listro, found himself up against the costly reality of group health insurance plans. As a growing organization, they knew they needed a competitive benefits package to attract and retain talent. But how could they achieve this without overstretching their budget?
The Quest for an Affordable Solution
Upon exploring various options, Joey stumbled upon the QSEHRA. As the only full-time staff member, traditional employer plans were prohibitively expensive, costing nearly five times more than a QSEHRA.
But the unfamiliarity of QSEHRA presented its own hurdles. Joey's board of directors had never heard of it and were unsure about its legality. As a non-profit, the board needed to approve the QSEHRA, meaning Joey had to provide accurate information to get everyone on the same page.
Enter Take Command
That's where Take Command stepped in, offering guidance and educational resources about QSEHRA. With this support, Joey was able to clarify the benefits of QSEHRA to his board, gaining their approval to move forward with the setup.
Take Command’s team continued to assist Joey throughout the setup process, providing a simple, user-friendly platform for managing the QSEHRA. As a result, New Britain ROOTS successfully implemented their QSEHRA in January, currently reimbursing premiums only.
Joey shares, "The setup was quick and simple, and reporting and reimbursements are easy as well."
The Impact of QSEHRA
By implementing QSEHRA, New Britain ROOTS could afford to provide health benefits to its small team. Moreover, this choice allowed them to remain competitive in the job market, a crucial factor as they plan to expand their team.
This case study exemplifies how nonprofits, even with limited resources, can leverage QSEHRA to provide affordable, sustainable health benefits to their team, supporting their mission and growth.
Individual Coverage Health Reimbursement Arrangement (ICHRA)
What are ichras.
The Individual Coverage Health Reimbursement Arrangement, or ICHRA, is a type of HRA that allows employers to reimburse employees for individual health insurance premiums and eligible medical expenses on a pre-tax basis. Unlike the QSEHRA, ICHRA has no annual contribution limits, and employers can offer ICHRAs to different classes of employees, with varying contribution amounts.
The Advantages of ICHRAs for Nonprofits
ICHRA presents several distinctive advantages to nonprofits, transforming the way these organizations provide health benefits to their employees:
- Flexibility and Customization: Perhaps the most significant advantage of ICHRAs is the flexibility they provide. Nonprofits can customize their contributions based on distinct employee classifications such as full-time, part-time, seasonal employees, or even based on geographic location. This means nonprofits can offer a competitive benefits package that matches the diverse needs of their workforce.
- Cost Control: Budgeting is a major concern for most nonprofits, and the predictability of ICHRAs makes them an attractive option. Organizations can set defined contribution amounts, thus effectively managing their healthcare expenditure. This allows for better financial planning and resource allocation without the fear of escalating health insurance premiums.
- No Size Limitation: Unlike QSEHRAs, which are exclusive to employers with fewer than 50 employees, ICHRAs are accessible to nonprofits of any size. This scalability makes ICHRA a feasible health benefit solution for a wider range of organizations, from small local charities to large national nonprofits.
- Tax Advantages: The tax benefits offered by ICHRAs cannot be overlooked. Reimbursements provided through an ICHRA are not considered taxable income for employees, making them a more attractive benefit. Simultaneously, these reimbursements are tax-deductible for the nonprofit, leading to substantial tax savings.
- Employee Choice: ICHRAs empower employees with greater choice and autonomy over their healthcare decisions. They can select the individual health insurance that best meets their needs and that of their families. This can lead to higher satisfaction levels and increased loyalty among employees.
Limitations of ICHRAs for Nonprofits
While ICHRAs offer numerous benefits, it's important to also consider potential limitations. This balanced perspective ensures that your nonprofit makes an informed decision that aligns with its specific circumstances, resources, and the needs of its workforce. In this section, we'll delve into the challenges that ICHRAs may pose and how they can be effectively addressed.
- Employee Coverage Requirement: Employees must have individual health insurance coverage to participate in an ICHRA. This could be a limitation for employees who lack access to affordable individual health insurance options. However, Take Command can assist employees in finding the right insurance plan that aligns with their healthcare needs and financial capabilities
- Administrative Complexity: ICHRAs can be administratively complex to manage due to their customizable nature. Ensuring compliance with various regulations may require additional resources. But with Take Command's comprehensive HRA administration service, nonprofits can effectively manage their ICHRAs without the stress. We handle everything from setup, plan design, and compliance documentation, to employee education and ongoing support.
Leveraging ICHRAs for Nonprofits with Take Command: A Strategic Approach to Health Benefits
ICHRAs provide a flexible and scalable health benefits solution for nonprofits of all sizes. While they have some limitations, with proper administration, ICHRAs can be a strategic tool for nonprofits to attract and retain talent while managing their health benefit costs effectively.
By partnering with Take Command, nonprofits can fully leverage the benefits of an ICHRA while mitigating potential drawbacks. Our services ensure that ICHRAs become a strategic, manageable, and effective tool in your health benefits arsenal.
Health benefits for small nonprofits
Small nonprofits have an HRA designed specifically for them. It's called a Qualified Small Employer HRA and it's for nonprofits with less than 50 full time equivalent employees.
What are QSEHRAs?
QSEHRA is a specific type of HRA designed for small employers with fewer than 50 employees who do not offer a group health insurance plan. QSEHRA allows these employers to provide a set amount of tax-free money to their employees each year. Employees can use this money to purchase individual health insurance and cover other qualifying healthcare expenses.
The Advantages of QSEHRAs for Small Nonprofits
QSEHRAs bring several compelling benefits to the table for smaller nonprofits:
- Cost Control : In an economic climate where expenses need to be carefully managed, QSEHRAs provide nonprofits with predictable and controlled costs. Nonprofits can determine their own annual budget for health benefits, providing financial certainty that is especially crucial for smaller organizations operating on limited budgets.
- Simplicity and Ease of Management: QSEHRAs offer a simpler structure compared to their ICHRA counterparts. With fewer customization options and regulations, the administrative burden for small nonprofits is significantly reduced. This simplicity makes QSEHRAs an excellent choice for organizations with limited administrative capacity or those just starting to offer health benefits.
- Tax Benefits: The tax advantages of QSEHRAs are a win-win for both nonprofits and their employees. Nonprofits can deduct their contributions from their taxes, thereby reducing their overall tax liability. On the other hand, employees receive these reimbursements tax-free, maximizing the value of their health benefits.
- Employee Empowerment: With QSEHRAs, employees have the flexibility to choose their own health insurance plan that suits their personal needs and circumstances. This autonomy can lead to higher satisfaction and engagement among employees, which is crucial for attracting and retaining talent in the nonprofit sector.
- Legal Compliance: QSEHRAs are fully compliant with the Affordable Care Act (ACA) rules, removing the risk of penalties and ensuring legal conformity. This compliance reassurance further adds to the appeal of QSEHRAs for small nonprofits.
- Integration with sharing ministries: Nonprofits can reimburse employees for their sharing ministry costs with a QSEHRA as long as a Minimum Essential Coverage plan has also been set up.
These advantages position QSEHRAs as a highly suitable health benefits solution for small nonprofits, offering simplicity, cost control, tax advantages, and employee satisfaction.
Limitations of QSEHRAs for Nonprofits – And How Take Command Can Help
While QSEHRAs offer several unique benefits for smaller nonprofits, it's also important to be aware of their limitations:
- Employee Limitations: QSEHRAs are exclusively available to employers with fewer than 50 employees. Larger nonprofits seeking to leverage the benefits of an HRA would need to consider an ICHRA instead. However, for smaller nonprofits that qualify, Take Command simplifies the setup and administration process, making QSEHRAs an accessible and easy-to-manage solution.
- Contribution Limits: Unlike ICHRAs, QSEHRAs come with IRS-set annual contribution limits. These limits may restrict the extent of health benefits a nonprofit can provide. Fortunately, Take Command's platform allows organizations to easily track and manage their contributions, ensuring they remain within IRS guidelines while maximizing the value they can provide to their employees.
- No Customization: QSEHRAs do not permit nonprofits to differentiate contributions based on employee classifications. This one-size-fits-all approach might not be ideal for nonprofits looking for a more flexible benefits solution. With Take Command, however, nonprofits can leverage expert guidance and tools to design a comprehensive benefits strategy that takes into account the advantages of QSEHRAs, complemented by other benefit options as necessary.
20% of nonprofits lack employer-sponsored health insurance
Approximately 1 in 7 of our clients are nonprofits reimbursing their employees for health insurance with Individual Coverage HRAs (ICHRAs) and Qualified Small Employer HRAs (QSEHRAs) for small nonprofit health insurance.
Take Command Streamlines Nonprofit Health Benefits Management
Despite these limitations, partnering with Take Command can significantly streamline the process of implementing and managing a QSEHRA. Our comprehensive HRA administration service simplifies compliance, setup, and ongoing management, empowering small nonprofits to offer competitive health benefits despite resource constraints. In the long run, these benefits contribute to employee satisfaction, talent retention, and ultimately, the nonprofit's mission success.
Flexible Designs
No more one-size fits all plans! HRA plans for nonprofits can be customized and designed to achieve you or your clients’ goals and are more flexible with what types of plans they will reimburse.
Simple Administration
Take Command will automatically generate the documents your nonprofit employees need and can help them search for and enroll in a plan online.
On-Ramp to Benefits
80% of our small business clients are net new to benefits. An HRA is an affordable, simple way to offer scalable benefits to your team on your budget.
Comparison: HRAs vs. Traditional Group Health Plans for Nonprofits
When it comes to health benefits for nonprofits, understanding the advantages and considerations of different options is crucial. Let's compare HRAs, including ICHRAs and QSEHRAs, with traditional group health plans to help nonprofits make informed decisions.
Advantages of HRAs over Traditional Group Health Plans
- Cost Control: HRAs allow nonprofits to control costs by setting a fixed contribution amount. Traditional group health plans often come with higher premiums, making HRAs a cost-effective alternative.
- Flexibility: HRAs offer more flexibility in benefit design, allowing nonprofits to tailor reimbursement amounts and eligible expenses to better meet the unique needs of their employees.
- Tax Efficiency: HRAs provide tax advantages for both nonprofits and employees, with reimbursements typically being tax-deductible for the organization and tax-free for employees.
Examples of Non profit benefit packages
- HRAs (including ICHRAs): HRAs, with their cost control and flexibility, are particularly advantageous for nonprofits seeking a customized benefits approach. They work well for organizations with diverse employee classes, varying healthcare needs, and a desire to offer personalized benefits.
- Traditional Group Health Plans: Nonprofits with limited administrative resources and employees who prefer the simplicity and comprehensive coverage of a group plan may find traditional group health plans more suitable. This is especially true for smaller nonprofits without the capacity to manage the complexity of HRAs effectively.
Understanding the specific needs, resources, and preferences of your nonprofit is essential in selecting the most beneficial health benefits plan, whether it be an HRA or a traditional group health plan. Evaluating the advantages and potential limitations of each option can guide nonprofits in finding the right fit for their unique circumstances.
Comparison: HRAs for Nonprofits vs. Sharing Ministries
When it comes to health benefits for nonprofits, there are various options to consider. Let's compare Health Reimbursement Arrangements (HRAs), including ICHRAs and QSEHRAs, with Sharing Ministries to help nonprofits make informed decisions.
Advantages of HRAs over Sharing Ministries
- Cost Control: HRAs allow nonprofits to have control over their healthcare costs by setting a fixed contribution amount. In contrast, Sharing Ministries require members to contribute a monthly share, which may vary based on factors such as family size and medical history.
- Flexibility: HRAs offer more flexibility in benefit design. Nonprofits can tailor reimbursement amounts and eligible expenses to better meet the unique needs of their employees. Sharing Ministries often have specific guidelines on what expenses are eligible for sharing, which may limit flexibility.
- Tax Efficiency: HRAs provide tax advantages for both nonprofits and employees. Nonprofits can typically deduct their HRA contributions from their taxes, reducing their overall tax liability. Employees receive HRA reimbursements tax-free, maximizing the value of their health benefits. Sharing Ministries, on the other hand, are not subject to the same tax advantages.
Examples of Beneficial Plans for Nonprofits
- HRAs (including ICHRAs): HRAs provide cost control, flexibility, and tax advantages, making them advantageous for nonprofits seeking a customized benefits approach. They are well-suited for organizations with diverse employee classes, varying healthcare needs, and a desire to offer personalized benefits.
- Sharing Ministries: Sharing Ministries can be a viable option for nonprofits that prioritize community, simplicity, and broader coverage. They may be suitable for organizations with employees who share a common faith and value a faith-based approach to healthcare.
Understanding the specific needs, values, and preferences of your nonprofit is essential in selecting the most beneficial health benefits plan. Evaluating the advantages and potential limitations of each option, whether it be an HRA or a Sharing Ministry, can guide nonprofits in finding the right fit for their unique circumstances.
Making the Choice: Best Health Benefits for Nonprofits
When it comes to selecting the best health benefits plan for your nonprofit, several factors should be taken into consideration. By carefully evaluating these factors, you can make an informed decision that aligns with your organization's size, financial capacity, and the specific needs of your employees.
Factors to Consider When Choosing a Health Benefits Plan
- Size of Organization: The size of your nonprofit plays a significant role in determining which health benefits plan is most suitable. Smaller organizations may find traditional group health plans more manageable, while larger organizations can take advantage of the flexibility offered by HRAs, such as ICHRAs or QSEHRAs.
- Financial Capacity: Assessing your nonprofit's financial resources is crucial. HRAs provide cost control and predictable budgeting, making them attractive for nonprofits with limited financial capacity. Traditional group health plans may require more substantial financial investment but can offer comprehensive coverage.
- Specific Needs of Employees: Understanding the unique needs and preferences of your employees is essential. Consider factors such as demographics, healthcare requirements, and the value they place on choice and flexibility. This information can help determine whether HRAs or traditional group health plans are a better fit.
Guidelines for Choosing the Most Suitable Plan
- Evaluate Cost and Budget: Carefully analyze the costs associated with each health benefits plan, including premiums, contributions, and potential out-of-pocket expenses for both the nonprofit and employees. Consider the long-term financial sustainability and alignment with your nonprofit's mission.
- Assess Employee Preferences: Survey your employees to understand their preferences and needs regarding healthcare coverage. Consider their desire for choice, flexibility, and the value they place on comprehensive coverage versus cost-sharing.
- Seek Expert Guidance: Consult with benefits advisors, insurance brokers, or HR professionals who specialize in nonprofit health benefits. Their expertise can provide valuable insights and help navigate the complexities of different plan options.
- Consider Compliance and Administration: Evaluate the administrative requirements and compliance responsibilities associated with each plan. Assess your organization's capacity to handle the necessary paperwork, reporting, and legal obligations. If needed, consider partnering with a health benefits administration service like Take Command Health for streamlined administration and compliance support.
By carefully considering these factors and following these guidelines, nonprofits can choose the health benefits plan that best suits their organization's size, financial capacity, and the specific needs of their employees. Making an informed decision ensures that your nonprofit can provide valuable, competitive health benefits that support your employees' wellbeing while aligning with your mission and financial goals.
Navigating Employee Benefits for Nonprofits: Requirements, Exemptions, and Tax Credits Explained
Nonprofits are not generally required by law to offer benefits to their employees. However, there are certain requirements and exemptions to consider in the context of nonprofit organizations and their employee benefits. Let's explore these aspects further:

Are nonprofits required to offer benefits?
Nonprofits are not mandated to provide employee benefits, such as health insurance, by federal law. Unlike many for-profit companies subject to the Affordable Care Act's employer mandate, nonprofits are generally exempt from this requirement. However, it's important to note that state laws and regulations may vary, so nonprofits should consult local regulations to ensure compliance.
Are there exemptions for Nonprofits?
Nonprofits may qualify for certain exemptions and alternatives when it comes to employee benefits. For example, some religiously affiliated nonprofits may be exempt from certain contraceptive coverage requirements based on religious objections. It's crucial for nonprofits to understand their legal obligations and any exemptions that may apply to their specific circumstances.
Are there tax credits for nonprofits?
While nonprofits may not be subject to the same tax credit programs as for-profit businesses, there are tax incentives and credits available to help offset costs associated with employee benefits. For instance, the Small Business Health Care Tax Credit is available for eligible small employers, including nonprofits, that provide health insurance coverage to their employees. Nonprofits should consult with tax professionals or benefits advisors to explore potential tax credits and incentives specific to their organization.
It's important for nonprofits to carefully navigate the legal landscape and understand the specific requirements and exemptions related to employee benefits. Consulting with legal and tax advisors who specialize in nonprofit organizations can provide valuable guidance and ensure compliance with applicable laws and regulations. Additionally, exploring tax credits and incentives can help nonprofits mitigate costs associated with providing employee benefits, further supporting their financial sustainability and mission-driven objectives.
Guiding Nonprofits towards the Right Health Benefits Plan with Take Command
Providing health benefits for nonprofits is a critical aspect of attracting and retaining top talent while promoting the wellbeing of employees. However, navigating the complexities of health benefits can be challenging for these organizations. In this article, we have explored the potential solutions offered by HRAs, including ICHRAs and QSEHRAs, for nonprofits. HRAs provide several benefits for nonprofits, such as cost control, flexibility, and tax efficiency.
ICHRAs offer customization and scalability, while QSEHRAs are suitable for smaller organizations seeking simplicity. These HRAs empower nonprofits to design personalized benefits that align with their financial capacity and the specific needs of their employees.
Throughout the decision-making process, nonprofits should carefully evaluate their unique needs and circumstances. Factors such as organization size, financial capacity, and employee preferences should be considered when selecting a health benefits plan. Seeking guidance from experts in the field and leveraging trusted partners like Take Command can provide nonprofits with the knowledge and support needed to make informed decisions.
Take Command offers comprehensive services to help nonprofits navigate the complexities of HRAs, ensuring compliance, simplifying administration, and providing personalized guidance. With their expertise, nonprofits can maximize the benefits of HRAs while mitigating potential drawbacks, enabling them to offer competitive health benefits that contribute to the overall success of their mission.
Our experienced and friendly team is ready to help you on your health benefits journey.
How much will you save with a QSEHRA?
Since QSEHRA reimbursements are tax-free, small business owners can enjoy considerable savings. Check out our QSEHRA tax savings calculator to get a savings estimate.
QSEHRA rules
QSEHRA rules for employers and employees include some standard HRA rules associated with every HRA account. For example, the business owns the HRA, not the employee. Only the company can put money into the HRA, HRA funds do not earn interest, and the business determines the amount contributed to the HRA.
Employees can use QSEHRA money to pay for personal and family medical expenses. The rules for reimbursement from a QSEHRA are found in IRS Publication 502 , and any unused money stays with the business. Rollover of funds for employees with a QSEHRA is not guaranteed. Rollover depends on the type of plan and the business's decision about allowing it or not.
→ Deep dive into HRA Account Rules
What are the QSEHRA rules and 2023 QSEHRA limits?
Businesses with fewer than 50 employees can contribute a maximum of $5,850 for individual employees and a contribution of $11,800 for employees with a family. This is an increase over the QSEHRA 2022 limits! Compared to QSEHRA limits 2023, 2023 QSEHRA limits have increased by $400 for individual employees and $750 for employees with a family annually.
Offering personalized benefits for your small business is possible with Take Command. Our qualified small employer health reimbursement arrangement administration software makes QSEHRA administration simple and easy.
Here’s what you can expect from your QSEHRA when you work with a skilled HRA administrator like Take Command.
Flexible Designs: Customize a plan that fits the needs of you and your mixed workforce employees. Employers can choose different reimbursement amounts for each employee class based on different class distinctions.
Simple Administration: Take Command helps you with the design and management of your QSEHRA. This includes process, compliance, reporting, employee communication, and employer support. We’ll ensure you know the QSEHRA rules, 2023 QSEHRA limits, and what QSEHRA funds can be used for.
No Minimum Contribution Requirements: You can offer different reimbursement allowances based on family status and there are no minimum 2023 QSEHRA limits or minimum contribution requirements, only a maximum limit.
Tax-advantaged: QSEHRA is completely tax-free for employers and tax-free for employees with minimum essential coverage (MEC).
Begin designing your QSEHRA plan today and be set up in minutes
You could start reimbursing your employees tax-free sooner than you think.
QSEHRA requirements
To set up a QSHERA, a small business must meet two QSEHRA requirements to be eligible. The employer QSEHRA requirements are:
- Be “small”: The business or non-profit must be a “small employer” in the eyes of the IRS, meaning it must have 50 or fewer full-time employees to meet QSEHRA eligibility.
- Not have a group health plan: The small business or non-profit cannot have a traditional group health plan.
To qualify for QSEHRA tax-free reimbursements, employees must meet two QSEHRA requirements to be eligible:
- Have individual health insurance coverage. Plans must provide Minimum Essential Coverage (MEC) as defined by the IRS in Section 106(g).
- Submit claims for reimbursement. Employees need to prove their expenses met the QSEHRA requirements for qualified health expenses.
ICHRA vs QSEHRA
ICHRA and QSEHRA are both awesome tax-advantaged tools to consider when searching for a small business health insurance solution for your company. There are a few key differences, like what kind of business qualifies, reimbursement limits or maximums, employee eligibility, and more. Here’s a helpful blog complete with a side-by-side comparison of ICHRA vs QSEHRA.
See the chart ICHRA vs QSEHRA.
QSEHRA pros and cons
There are always upsides and downsides to consider when deciding which healthcare plan to choose. It really depends on the specifics of your situation and the plan you choose. Let’s review some of the general pros and cons of QSEHRA plans.
In a nutshell, there are way more pros than cons to QSEHRA. Here’s a few.
- Tax efficiency
- Flexible design
- Budget control
- Optimized benefits
- You can get out of the health insurance risk management game
Advantages of QSEHRA plans:
Cost savings: Employers control how much is spent on health coverage and decide the maximum reimbursement allowances. And any u nused HRA account funds can roll over at the employer's discretion annually; otherwise, the funds stay with the employer.
Tax advantages: Tax benefits for employers and employees. Employers can deduct reimbursements made to employees through QSEHRA, reducing their overall tax liability. And reimbursements given to employees through QSEHRA are not considered taxable income, so employees won’t have to pay taxes on reimbursements.
Greater plan flexibility: Employers can customize the plan and choose the type of coverage they want to offer, the amount of the reimbursement, and the eligibility requirements. Employers can also choose to offer different levels of coverage to different classes of employees .
Health benefit choice: Employees choose the individual plans and doctors that work best for them and can use QSEHRAs for medical and dental expenses, prescriptions, annual exams, birth control medications, and more.
Risk de-management: Employers no longer need to worry about factoring managing employees’ health risks into the business strategy.
Plan portability: Employees can keep their individual health insurance plan and don’t have to lose health coverage tied to a specific job.
ACA compliance: QSEHRA also helps employers comply with the Affordable Care Act (ACA). The plan meets the ACA’s minimum requirements for employer-sponsored health plans, allowing employers to avoid potential penalties.
Administration simplicity: QSEHRA doesn’t require employers to manage a large group insurance plan, which can save employers time and money by streamlining their administrative processes.
Potential QSEHRA Disadvantages
Non-transferable funds: QSEHRA funds stay with the employer if the employee leaves the company. The good news is that the employee keeps the health insurance plan they selected.
Cosmetic procedures not covered: Elective cosmetic procedures like teeth whitening aren’t covered. Most group plans don’t cover elective cosmetic procedures, either.
Limited coverage: Provider options may be limited based on the insurance market per geographical region.
QSEHRA eligible expenses
When you set up your QSEHRA, you’ll want to ensure your employees know what qualifies for QSEHRA reimbursement. QSEHRA-eligible expenses include a variety of things that may include a health insurance premium, prescription and non-prescription drugs, personal hygiene products, doctor visits, dental and vision care, mental health care, and more, as long as the employee has minimum eligible coverage (MEC). Make sure that the expenses follow the guidelines by IRS Publication 502 Medical and Dental Expenses.
Here’s a full list of QSEHRA-eligible expenses for employees in 2023.
How to set up a QSEHRA
When you work with a QSEHRA third-party administrator like Take Command, we ensure your QSEHRA administration is straightforward and simple. Sure, you could do a self-administered QSEHRA, but without a skilled HRA administrator in your corner – that includes things to make it easy on you, like QSEHRA administration software and QSEHRA plan document template – you’re in for a lot of work and headaches.
So, pro tip, go with a QSEHRA third-party administrator when thinking about how to set up a QSEHRA.
Here’s how to set up a QSEHRA.
Employees select their preferred health insurance plan, pay for health care expenses upfront then the employer reimburses them. Employers can offer health care benefits without being tied to a group plan and employees gain control of where they spend their money and chose the providers that they want.
How to set up QSEHRA in 4 simple steps
- The employer designs their QSEHRA plan. Pro tip – it’s even easier when you work with an experienced partner like Take Command.
- Employees purchase their preferred health insurance plan. Take Command even helps them do it and makes it super easy with tons of employee resources , including our window shopping tool.
- After employees purchase their plans of choice, they can then submit eligible reimbursement claims to the employer.
- The employer reimburses employees for all valid reimbursement claims.
Let's talk through your HRA questions
Fill out the form below to connect with our team and see if an HRA is a good fit.

Susanne is a copywriter specializing in the health and wellness industry. Before starting her own business, she spent nearly a decade at a marketing agency doing all of the things – advisor, copywriter, SEO strategist, social media specialist, and project manager. That experience gives her a unique understanding of how the consumer-focused content she writes flows into each marketing piece. Susanne lives in Oklahoma City with her husband and two daughters. She loves being outdoors, exercising and reading.
We’re on a mission to create a consumer-centric healthcare system.
(855) 824-4727
©2024 Take Command. All Rights Reserved.
Take Command Health is a financial technology company, and is not a bank. Banking services are provided by Blue Ridge Bank and TransPecos Banks, Members FDIC. FDIC insurance is available for funds on deposit up to $250,000 through Blue Ridge Bank Member FDIC or TransPecos Banks, Member FDIC. Please refer to your Deposit Agreement to confirm your Bank Partner.
Privacy Policy Terms of Use Licensing Sitemap Secured with SSL
HERE’S WHAT EVERY NONPROFIT SHOULD KNOW ABOUT OFFERING HEALTH INSURANCE

Get in touch
- 800.442.4867
- [email protected]
- Newsletter Signup
- 501(c) Agencies Trust
- 501(c) HR Services
- 501(c) Unemployment Assist
- Boy Scouts Unemployment Plan
- Native Freedom Trust
- First-Dollar
- WA State Worker’s Comp
- Reimbursing 101
© 2024 501(c) Services. Legal/Privacy Policy | Website by Outmark
- WA State Workers’ Compensation
- State Unemployment Insurance Reimbursing Explained
- Benefits and Risks
- Unemployment Reimbursing Options
- Resource Library
Keep up with the news
Subscribe to our monthly newsletter for timely updates, news, and events.

- Book a Speaker
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Vivamus convallis sem tellus, vitae egestas felis vestibule ut.
Error message details.
Reuse Permissions
Request permission to republish or redistribute SHRM content and materials.
When do group health plan benefits terminate for an employee on a non-FMLA leave of absence?
Continuation of group health plan benefits during periods of leave may depend on the type of leave an employee is on. When an employee is on Family and Medical Leave Act (FMLA) leave, a covered employer is required to maintain group health insurance coverage for an employee and his or her family under the same terms and conditions held prior to the leave. However, when an employee is not on FMLA leave, an employer may need to determine if the leave falls under other federal or state leave laws.
Some states have leave laws that provide time off similar to the federal FMLA leave. For example, Wisconsin has its own family and medical leave law that has different eligibility requirements from the federal FMLA. An employee could be eligible for Wisconsin Family and Medical Leave Act leave but not for FMLA leave. When an employee is on Wisconsin FMLA leave, health insurance should continue under the same conditions as for active employees. Employers should review applicable state leave laws to determine obligations to continue benefits during periods of leave.
If an employee is on leave as a reasonable accommodation under the Americans with Disabilities Act (ADA), an employer must continue an employee's health insurance benefits during the leave if it does so for other employees on similar leave. For example, if an employee is permitted to continue health benefits during periods of unpaid, personal leave, an employee on unpaid leave under the ADA should be able to continue health benefits too.
The Pregnancy Discrimination Act (PDA) does not provide leave benefits, but it does require employers to treat employees the same as other temporarily disabled employees with regard to benefits. Therefore, if an employer allows an employee to take leave due to a temporary disability and that employee is permitted to maintain health benefits during that leave, an employee on leave due to pregnancy must also be permitted to maintain health benefits while on leave.
If an employee is not eligible for federal or state leave but is eligible for an employer-provided leave of absence, the continuation of health benefits is based on the language in the benefits plan. An employee may continue health benefits during periods of employer-provided leave as allowed by the insurance plan documents and approved by the health plan insurer. Employers should address in the written plan documents how long an employee can be absent from work on unprotected leave before health benefits will be terminated and ensure these plan rules are followed consistently.
If benefits are not continued, an employee may elect health care continuation under COBRA due to the qualifying event of a reduction in hours.
Related Content

Why AI+HI Is Essential to Compliance
HR must always include human intelligence and oversight of AI in decision-making in hiring and firing, a legal expert said at SHRM24. She added that HR can ensure compliance by meeting the strictest AI standards, which will be in Colorado’s upcoming AI law.

A 4-Day Workweek? AI-Fueled Efficiencies Could Make It Happen
The proliferation of artificial intelligence in the workplace, and the ensuing expected increase in productivity and efficiency, could help usher in the four-day workweek, some experts predict.
Advertisement

Artificial Intelligence in the Workplace
An organization run by AI is not a futuristic concept. Such technology is already a part of many workplaces and will continue to shape the labor market and HR. Here's how employers and employees can successfully manage generative AI and other AI-powered systems.
HR Daily Newsletter
New, trends and analysis, as well as breaking news alerts, to help HR professionals do their jobs better each business day.
Success title
Success caption
How nonprofits can offer health insurance
Health Benefits • January 19, 2023 at 9:20 AM • Written by: Chase Charaba
Share article
As healthcare costs rise each year, small and midsize employers sometimes struggle to deliver quality health benefits to their employees. This can be especially true for nonprofit organizations since revenue can vary significantly from month to month.
In a PeopleKeep survey of nonprofit business owners, 81% said that cost was one of the most pressing challenges in finding a healthcare plan that fits their needs. Additionally, more than half of those surveyed said they’re interested in seeing the federal government expand the number of alternatives to traditional group coverage .
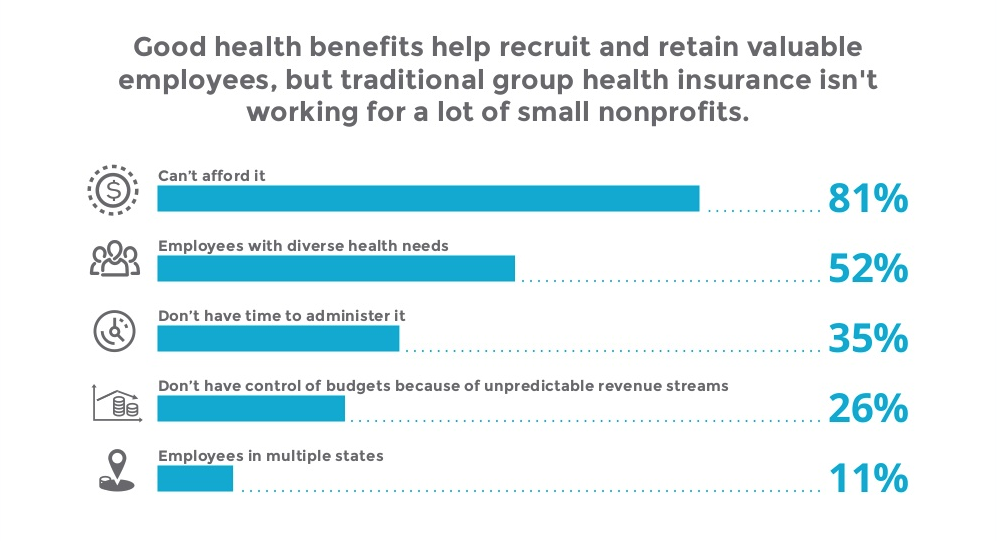
Luckily, there are alternatives to traditional group health insurance plans that many nonprofits have found instrumental in offering quality health benefits to their workers.
This article will cover how nonprofits can offer affordable health benefits and why these alternatives to traditional group health insurance work for nonprofit organizations.
Get our comprehensive guide on offering health benefits as a nonprofit
What health insurance benefits are available to nonprofit organizations?
There are various ways nonprofit organizations can offer health benefits to their staff. While small group health insurance options are available, many small businesses and nonprofits find it challenging to offer these medical plans to their workers due to the cost and complexity associated with traditional group health insurance.
Popular alternatives include health reimbursement arrangements (HRAs) and employee stipends . We’ll cover these options in-depth in the sections below.
What is a health reimbursement arrangement (HRA)?
An HRA is an IRS-approved, employer-funded health benefit used to reimburse employees for qualifying out-of-pocket medical care expenses and individual health insurance premiums.
Many for-profit companies and nonprofits use HRAs over group health insurance or health stipends because of the tax advantages and budget control that HRAs facilitate compared to an insurance agency.
With an HRA, organizations set a monthly allowance for employees to use. After making a wide range of eligible healthcare purchases, including insurance premiums, employees submit documentation of their medical expenses to their employer.
From there, you’ll review the documents and reimburse employees up to their monthly allowance amount, tax-free, if everything’s in order.
There are a few different types of HRAs, each with its own features and requirements that enable nonprofit organizations to deliver meaningful benefits to their employees.
Qualified small employer HRA (QSEHRA)
First up is the qualified small employer HRA (QSEHRA). A QSEHRA is specifically designed for organizations with fewer than 50 full-time equivalent employees (FTEs).
With a QSEHRA, all eligible reimbursements are free of payroll tax for the organization and its employees. Reimbursements can also be free of income tax for employees if the employee has medical coverage through a policy providing minimum essential coverage (MEC).
Individual coverage HRA (ICHRA)
Next, there’s the individual coverage HRA (ICHRA). Like a QSEHRA, nonprofits and other businesses can use an ICHRA to reimburse employees tax-free for individual health insurance premiums and other medical expenses.
All employers with at least one W-2 employee can offer an ICHRA. This includes businesses, nonprofits, government entities, and religious organizations.
Unlike a QSEHRA, an ICHRA can be offered by organizations with 50 or more full-time employees. You can also use it to satisfy the Affordable Care Act (ACA)’s employer mandate as long as your workers have individual health insurance coverage that meets MEC.
An ICHRA can be offered as a stand-alone benefit or as another benefits option for your employees who don't qualify for your group health insurance policy. However, group health insurance and an ICHRA can't be offered together to the same group of employees.
For example, you could offer group health insurance to your full-time employees and an ICHRA to part-time employees. However, you can only offer full-time employees an ICHRA or group health insurance, not both.
While newer than QSEHRAs, ICHRAs are also growing in popularity. A survey conducted by the Kaiser Family Foundation 1 found that 88% of large employers favored ICHRAs as an alternative to group health insurance. Additionally, the HRA Council 2 found that ICHRA adoption among U.S. employers tripled from 2020 to 2022.
Integrated HRA
Finally, there’s the group coverage HRA (GCHRA). Often referred to as an integrated HRA, a GCHRA is an employer-funded medical reimbursement plan linked with a group health insurance plan—usually a high-deductible health plan (HDHP).
GCHRAs are only offered to those who participate in an organization’s group plan, as it’s an ancillary benefit intended to help employees with their deductible costs.
Employees can use their GCHRA allowance to get reimbursed for healthcare costs before their out-of-pocket maximum is met or for expenses that aren’t fully covered by the group plan, such as vision or dental expenses.
Why are HRAs a good choice for nonprofit organizations?
While HRAs are an excellent health benefits solution for organizations of all sizes and types, they have a few special perks that make them an even more attractive choice for nonprofit organizations.
Benefits on a budget
HRAs empower nonprofit owners to offer quality health benefits on a tight budget. Rather than suffering through high costs and annual rate hikes, HRAs allow nonprofit owners to set a specific budget that they can count on month-to-month and year-to-year.
What's more, while nonprofit owners may not be able to offer employees corporate-level salaries, offering a competitive benefit more than makes up for it. According to our 2022 Employee Benefits Survey Report , 82% of employees said the benefits package an employer offers is an important factor in whether or not they accept a job with the organization.
By offering quality benefits, you’ll be able to attract and retain employees despite a tight budget.
Flexible plans
Another substantial advantage HRAs have for nonprofit organizations is their flexibility. Each employee can use the benefit differently and can even sign up for an individual insurance plan that meets their unique healthcare needs. With the individual health insurance plan of their choice and an HRA, you can give your employees access to health services in their area no matter where they live.
When employees can choose their own insurance plan, they’ll have access to their preferred doctors and hospitals. This isn’t always the case with traditional group insurers.
Nonprofit organizations typically employ people with a strong dedication to the group's mission. Employees often span several demographics, including age , marital status, insurance status, and even the state they live in. No matter how your team varies, a single HRA can work for all of them as long as they are W-2 employees.
Quick and easy to administer
Finally, HRAs are quick and easy to set up and administer monthly, especially if you utilize an automated software solution like PeopleKeep. With our software services to help you make reimbursements and our award-winning customer support team to answer your questions, you'll only need a few minutes every month to administer your own HRA.
Time-saving tools like those available with PeopleKeep are beneficial for nonprofit directors who often wear many hats, leaving them with little extra time to spend researching and administering employee benefits.
Alternatives to HRAs
While HRAs are an excellent option for providing healthcare benefits to your workers, they may not work for everyone. For example, if you employ independent contractors who receive Form 1099 instead of a W-2, they aren't eligible for an HRA. Likewise, international workers can't take advantage of an HRA's tax-free status.
In addition, because HRAs provide tax-free reimbursements for medical care expenses, including individual health insurance premiums, employees must account for their HRA allowance and any premium tax credits they receive.
With a QSEHRA, this means reducing tax credits by the amount of your QSEHRA allowance. If you offer an ICHRA to your workers, they'll have to choose between their ICHRA or tax credits if the ICHRA isn't considered affordable.
In these unique situations, a health stipend might be a better option. A health stipend works like an HRA, where you can provide a monthly allowance for medical expenses. However, they are taxable for both the employer and the employee.
Health stipends also come with fewer regulations than an HRA. This enables you to expand your eligible expenses to cover additional benefits like wellness costs and mental health services.
HRAs and health stipends are great options for nonprofit organizations struggling with the costs, time requirements, and other limitations of group health plans. With these alternatives to traditional group health insurance, you can provide personalized benefits to employees without breaking the bank due to rate increases.
With an HRA, you can control the benefits costs, provide value to employees regardless of your organization's size or budget, and outsource administration requirements to a software provider.
If you're ready to offer health benefits for your nonprofit, PeopleKeep can help! Our HRA and employee stipend administration software makes it easy for organizations like yours to set up and manage their benefits in minutes each month.
Schedule a call with a personalized benefits advisor to see how personalized benefits can work for your nonprofit
This blog article was originally published on March 9, 2016. It was last updated on January 19, 2023.
1. https://www.kff.org/report-section/how-corporate-executives-view-rising-health-care-cost-and-the-role-of-government-findings
2. https://hracouncil.wildapricot.org/resources/Documents/2022_HRAC_Data_FullReport_Final.pdf
Ready to enhance your employee benefits with PeopleKeep?

Chase Charaba
Chase Charaba is the content marketing manager at PeopleKeep. He started with the company as a content marketing specialist in early 2022. Chase has written more than 350 blog posts for various companies and personal projects throughout his career. He’s worked for digital marketing agencies, in-house marketing teams, and as the editor for national award-winning high school and college newspapers. He’s also a YouTuber, landscape photographer, and small business owner.

TechBullion
Benefits of group health insurance for small businesses.

Running a small business involves juggling various responsibilities, from managing finances to ensuring customer satisfaction. One crucial aspect that can significantly impact your business’s success is providing health insurance for your employees.
Group health insurance offers numerous benefits, making it an essential consideration for small business owners. In this comprehensive blog post, we’ll delve into the many advantages of group health insurance, exploring how it can benefit both employers and employees.
What is Group Health Insurance?
Group health insurance is a policy purchased by an employer and offered to eligible employees and their dependents. This type of insurance is typically more affordable than individual plans because the risk is spread across a larger pool of policyholders.
Small businesses, usually defined as those with 1-50 employees, can greatly benefit from group health insurance plans, which often provide a range of medical services and additional options such as dental and vision coverage.
Benefits of Group Health Insurance
Let’s look in to the various benefits of a group health insurance:
Cost-Effectiveness
One of the most significant advantages of group health insurance is its cost-effectiveness. Premiums for group plans are generally lower than those for individual plans because the insurance company’s risk is spread across many policyholders.
Additionally, the cost of these premiums is often shared between the employer and employees, making it more affordable for everyone involved.
According to Investopedia, group health insurance is usually cheaper than individual plans because more people buy into the plan, spreading the risk and reducing costs.
For small businesses, this cost-effectiveness is a major benefit. Lower premiums mean that providing health insurance is more feasible, allowing small business owners to offer competitive benefits without breaking the bank. This can be particularly advantageous in industries where employee turnover is high, as comprehensive benefits can help retain valuable staff.
Attracting and Retaining Talent
In today’s competitive job market, offering group health insurance can give small businesses a significant edge. Employees are more likely to join and stay with a company that provides robust health benefits.
This increases employee loyalty and reduces turnover, which can be costly and disruptive to business operations. According to a study by the Society for Human Resource Management (SHRM), health insurance is one of the most critical benefits for employees, and offering it can significantly impact job satisfaction and retention.
By providing group health insurance, small businesses can attract top talent who might otherwise choose larger companies with more comprehensive benefits packages. This competitive edge is crucial for small businesses looking to grow and succeed in their respective markets.
Tax Benefits
Group health insurance plans come with significant tax advantages for both employers and employees. For employers, the cost of premiums paid for employees is generally tax-deductible, reducing the overall tax burden.
Employees also benefit as their contributions toward premiums are made with pre-tax dollars, which lowers their taxable income. This tax efficiency makes group health insurance an attractive option for small businesses looking to maximize their financial resources.
Furthermore, small businesses offering health insurance may qualify for the Small Business Health Care Tax Credit if they meet specific criteria. This credit can cover up to 50% of the premiums paid for employees’ health insurance, providing substantial financial relief to small business owners.
Comprehensive Coverage
Group health insurance plans typically offer a broad range of medical services, ensuring that employees have access to the care they need. These services often include doctor visits, hospital stays, emergency services, preventive care, and more.
Many plans also allow businesses to add options like dental and vision coverage, providing employees with a comprehensive healthcare package.
This comprehensive coverage is particularly beneficial for small businesses, as it ensures that employees receive the necessary medical attention without incurring significant out-of-pocket expenses. By offering extensive coverage options, small businesses can promote employee well-being and productivity.
Improved Employee Health and Productivity
With access to preventive care and necessary medical treatments, employees are healthier and more productive. Regular health check-ups and early detection of illnesses can reduce absenteeism and increase overall workplace productivity.
According to a report by the Centers for Disease Control and Prevention (CDC), healthy employees are more engaged and efficient, contributing to a better working environment.
Providing group health insurance also demonstrates that a business values its employees’ well-being, which can boost morale and job satisfaction. When employees feel cared for, they are more likely to be committed to their work and perform at their best.
Simplified Plan Management
Many insurance providers offer administrative support to small businesses, making it easier to manage employee benefits. These services can include handling claims, providing customer support, and offering online tools for managing the plan.
This support simplifies the process and allows business owners to focus on running their business.
By leveraging the expertise of insurance providers, small business owners can ensure that their employees receive high-quality healthcare without the added burden of complex administrative tasks. This streamlined management of health benefits can save time and resources, allowing small businesses to operate more efficiently.
Legal Compliance and Financial Protection
Offering group health insurance helps small businesses comply with the Affordable Care Act (ACA) requirements, avoiding potential penalties. Under the ACA, businesses with 50 or more full-time employees must provide health insurance that meets minimum essential coverage standards.
Even though small businesses with fewer than 50 employees are not mandated to offer health insurance, providing it can still offer legal and financial benefits.
Group health insurance also protects employees from high medical costs, providing financial security and peace of mind. For many employees, the fear of unexpected medical expenses can be a significant source of stress.
By offering comprehensive health coverage, small businesses can alleviate this concern and support their employees’ financial well-being.
Additional Benefits for Small Businesses
Beyond the direct advantages of cost savings, tax benefits, and improved employee health, group health insurance can offer additional benefits for small businesses. These include:
- Enhanced Company Reputation : Offering health insurance can enhance a company’s reputation as a caring and responsible employer. This can attract not only employees but also customers who value businesses that prioritize their workforce’s well-being.
- Customizable Plans : Many insurance providers offer customizable group health insurance plans that can be tailored to meet the specific needs of a small business and its employees. This flexibility allows businesses to choose the coverage options that best suit their budget and workforce requirements.
- Support for Families : Group health insurance plans often extend coverage to employees’ families, providing additional support and peace of mind. This can be a significant advantage for employees with dependents, making the business a more attractive place to work.
- Access to Wellness Programs : Many group health insurance plans include access to wellness programs that promote healthy lifestyles and preventive care. These programs can include fitness classes, smoking cessation programs, and mental health resources, further enhancing employee well-being.
- Reduction in Turnover Costs : High employee turnover can be costly for small businesses, both in terms of direct expenses related to recruiting and training new employees and the indirect costs associated with lost productivity. By offering group health insurance, small businesses can reduce turnover rates and retain experienced employees, ultimately saving money and improving operational stability.
In conclusion, the advantages of group health insurance for small businesses are clear. By providing affordable, comprehensive coverage, small businesses can attract and retain top talent, improve employee health and productivity, and enjoy significant tax benefits.
Additionally, offering group health insurance demonstrates a commitment to employee well-being, enhancing the company’s reputation and contributing to long-term success.
Don’t overlook the potential impact of group health insurance on your small business—it’s an investment that can yield substantial returns in terms of employee satisfaction, loyalty, and overall business growth .

Recommended for you

Trending Stories

MetaHub Finance Teams up with Mastercard to introduce the Debit Card: Bridging Crypto and Traditional Finance
MetaHub Finance is excited to announce the launch of the Debit Payment Card, issued...

How Tycobit Token Presale Could Make Millionaires Overnight!
In the dynamic world of cryptocurrency, a new player is making waves with its...

Elon Musk’s XAI94K approaches $24B value with new funding round
Elon Musk‘s artificial intelligence company, XAI94K, is expected to complete a funding round in...

Revolutionizing HR: Enhancing Employee Experience and Operations with Generative AI
Generative AI is emerging as a revolutionary tool in the realm of Human Resources...

Where to Buy Halloween Costumes: A Comprehensive Guide
Halloween is the perfect time to unleash your creativity and transform into your favorite...

Integrating Virtual Medical Assistants into Your Healthcare Facility: A Step-by-Step Guide
Virtual medical assistants, or VMAs, are changing how healthcare facilities function. These digital aids...

Gatreon Ventures Launches $1 Million Web 3 Fund to Support Innovative Startups
Gatreon Ventures, a venture capital firm, is excited to announce the launch of its...

From Good to Great: How to Build the Best Version of Your Personality
In today’s fast-paced world, the importance of personal development cannot be overstated. Building the...

How IoT Healthcare Software Development is Boosting Efficiency in Healthcare
The healthcare industry has seen tremendous changes brought about by the advancement of modern...

Meet Aria Ohlsson: From Aspiring Writer to Blogging Star
In the bustling world of social media, where it’s tough to tell what’s real,...

BNB Chain Launches Mindpress a Data Marketplace
BNB Chain has launched Mindpress, a new data marketplace to make trading digital assets...

Samsung Odyssey OLED G8 Receives Reviews and Awards From Reviewers
Samsung Odyssey OLED G8 has received reviews and awards from reviewers such as Forbes,...

A 1000-Day Journey: 5 Lessons from Building a Startup Across Continents
The past 1000 days have been an incredibly fulfilling journey of intense work and...

SAFLE identity wallet unveils roadmap and raises funds at a $77M valuation
Identity wallet project SAFLE has undergone a major overhaul under the leadership of Apoorv...

The Best Presale Crypto / Journey to Crypto Presales/ Artemis Crypto Leads the way
The digital currency market has been going through a lot of growth and development...

AI Platform Stealing Uniswap Market Share Has Already Exceeded 50,000 Users, Here’s Why It Could Challenge Binance
A cutting-edge AI-powered trading platform is causing a stir, posing a challenge to key...

Digido: Quick and Easy Personal Loans in the Philippines
Are you in need of quick cash in the Philippines but tired of the...

The Future of Green Energy: How Pse.USDT Integrates Blockchain with Solar Power
In today’s globalized environment, Pse.USDT has emerged as a rising star by uniquely combining...

BlockDAG’s Victory Lap: Outselling Cardano & The Graph With A Whopping 12 Billion Coins
In the turbulent seas of the cryptocurrency market, a few names consistently capture the...

Hook Readers with the Perfect Ad Banner Design
Feeling stuck on how to make your ad banners stand out? You’re not alone....
Like Us On Facebook
Latest interview.

Rajendra Jakku, Information Security Specialist for a Leading Global Financial Institution, Implements AI Tools to Strengthen Internal Controls and Protect Data and Assets
Rajendra Prasad Jakku is Vice President, Information Security Specialist at one of the world’s leading financial institutions, where he heads Identity and...
Latest Press Release

View from the CEO: The emerging role of the Chief Data Officer
The volume of data that businesses are managing is increasing exponentially, with 329 trillion megabytes of data being created every day, according...
Pin It on Pinterest
- Circuit Courts Extend Non-Discrimination Protections for Transgender Individuals

On May 13, 2024, the Eleventh Circuit Court of Appeals held that certain federal non-discrimination protections apply to transgender individuals in the group health plan (insured and self-insured) context. In particular, the decision creates a significant new pathway for plan participants to challenge a plan’s limitations on coverage for gender-affirming care. This decision follows a similar April 29, 2024 decision in the Fourth Circuit. Plan sponsors, insurers, and third-party administrators should consider evaluating plans’ coverage exclusions and restrictions in light of these decisions.
Group health plans, plan sponsors, third party administrators, and health insurance issuers face increasing non-discrimination requirements. In 2024 alone, there have been many notable legal developments in these rules. Specifically, in May, the Department of Health and Human Services (“HHS”) released regulations under Affordable Care Act (“ACA”) section 1557 and Rehabilitation Act of 1973 section 504. Together, these rules prohibit entities that receive federal financial assistance from discriminating against individuals who are members of a recognized protected class (i.e., race, color, national origin, sex, disability, and age). Notably, the section 1557 final rule added the term “gender identity” to its description of sex discrimination. HHS explained in the preamble that “gender identity” is intended to “encompass ‘transgender status.’” [See our prior alert on section 1557 here and section 504 here .]
Most group health plans and health insurance policies in the group and individual markets are also subject to MHPAEA, which requires that plans offer mental health or substance use disorder benefits (“MH/SUD”) comparably with medical/surgical (“M/S”) benefits, meaning the plan cannot impose less favorable benefit limitations on MH/SUD benefits. Thus, under MHPAEA, plans that cover care related to gender dysphoria, a recognized mental health diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (“DSM”) V, must offer such benefits in parity with M/S benefits.
GROOM INSIGHT: The cases in the Eleventh and Fourth Circuits are some of the first cases addressing the interplay of federal non-discrimination rules and coverage of gender affirming care, with numerous cases pending in both district and appellate courts. [1] As a result, there exists a material potential for a circuit split, which over time could be considered by the Supreme Court. As part of this larger trend around the offer and provision of gender-affirming care, the Supreme Court agreed on June 24, 2024 to consider whether state-level prohibitions on the provision of gender-affirming care to minors are permissible. See U.S. v. Jonathan Skrmetti et al ., case number 23-477, in the Supreme Court of the United States. Thus, these cases represent an initial set of authority on the scope of federal nondiscrimination provisions that could impact the coverage of gender-affirming care for employers, the group health plans they sponsor, third-party administrators, and health insurance issuers.
The eleventh circuit decision’s implications.
In Lange v. Houston County, Georgia , the Eleventh Circuit found that the county’s group health plan’s exclusion for gender-affirming care caused the county to violate Title VII of the Civil Rights Act of 1964 as the sponsor of the plan. [2]
A transgender individual was employed by Houston County, in Georgia, and covered under its group health plan. She brought suit against the plan for its failure to cover gender-affirmation surgery. The plaintiff argued that the plan’s coverage exclusion for “sex change surgery” violated Title VII, the Americans with Disabilities Act (“ADA”), the Equal Protection Clause of the Fourteenth Amendment, and the equal protection guarantee under the Georgia Constitution. At summary judgment, the district court agreed as to the plaintiff’s Title VII claim, finding the group health plan’s coverage exclusion discriminated against plaintiff by limiting her “compensation, terms, conditions, or privileges of employment” on account of sex. In doing so, the court applied the Supreme Court’s 2020 decision in Bostock v. Clayton County, which held that discrimination based on sexual orientation or gender identity is prohibited under Title VII. The court determined, however, that the plaintiff alleged insufficient evidence to support the ADA claim. The court did not issue a decision on the merits as to her equal protection claims, but noted these claims may proceed to trial to the extent plaintiff seeks prospective relief. The district court explained, “the implication of [the U.S. Supreme Court’s] Bostock [decision] is clear. . . [a]n individual’s . . . transgender status is not relevant to employment decisions . . . discrimination on the basis of transgender status is discrimination on the basis of sex and is a violation of Title VII.” The district court also issued a permanent injunction preventing the county from enforcing its gender-affirmation surgery exclusion and directed the group health plan to process the plaintiff’s previously denied claim related to gender-affirming care.
On review, the Eleventh Circuit agreed that the plan violated Title VII but did not consider the ADA or equal protection claims. The court reasoned that plan violated Title VII because it denied the appellee’s healthcare claim “because the employee is transgender.” The court explained that the district court properly applied precedent from Bostock v. Clayton County , finding the plan’s denial of coverage for gender affirming care “deprived [plaintiff] of a benefit or privilege of her employment by reason of her nonconforming traits, thereby unlawfully punishing her for her gender nonconformity.” The court further explained that discriminating against transgender healthcare services equates to discriminating against a transgender individual since “sex is inextricably tied to the denial of coverage for gender-affirming surgery.” The court additionally cited the Equal Employment Opportunity Commission’s (“EEOC”) Title VII guidance and placed weight on the fact that the agency exercised its expertise by including protections for gender identity.
Notably, the Eleventh Circuit addressed the appellant’s argument that the cost of coverage of gender-affirming care would be burdensome to the group health plan. The court explicitly noted that, when a plaintiff establishes an injury resulting from a facially discriminatory practice, a group health plan cannot rely upon cost savings to justify its policy. The court concluded that after consideration of the balance of hardships, it was appropriate to find that appellee had established that the balance weighs in her favor.
On June 4, 2024, the defendants in Lange requested a rehearing before the entire Eleventh Circuit, which may be filed by a petition for a writ of certiorari before the Supreme Court.
GROOM INSIGHT: The Lange case presents a notable development in non-discrimination law under Title VII for employers offering group health plans. The liability in these cases is based on employment discrimination, not on group health plan compliance, so employers should assess their benefit designs to determine whether or not any plan limitations or exclusions facially discriminate against transgender individuals under Title VII – or could act as a subterfuge for otherwise prohibited discrimination.
Groom insight: the eeoc recently issued an opinion prohibiting opm from categorically excluding gender-affirming services from coverage under its group health plan. the eeoc found that the denial of gender-affirming care constitutes disparate treatment discrimination under title vii. the eeoc further noted that, while title vii does not necessarily require overage of all gender-affirming care, the statute prohibits healthcare coverage decisions that are based on protected characteristics. while this decision does not directly impact private employers, the eeoc’s reasoning will almost certainly extend to the private sector., the fourth circuit decision’s implications.
In Maxwell Kadel v. Dale , a decision decided by the full panel of judges on the Fourth Circuit, the court affirmed two district court decisions and ordered West Virginia and North Carolina to terminate coverage exclusions for gender-affirming care, explaining these exclusions constitute sex discrimination against transgender enrollees. [3]
West Virginia’s Medicaid Program covered some gender-affirming care, but excluded gender-affirming surgery. Similarly, North Carolina offered health coverage to its state employees but excluded “[t]reatment or studies leading to or in connection with sex changes or modifications and related care.” Transgender individuals whose plans denied health care related to their gender dysphoria brought suit. Both sets of plaintiffs sued under the Equal Protection Clause. The West Virginia plaintiffs additionally brought discrimination claims under the Medicaid Act and ACA section 1557. The district courts granted summary judgement in the plaintiffs’ favor and enjoined the states from enforcing these coverage exclusions.
The Fourth Circuit affirmed the district courts’ decisions and reasoned that plans that exclude treatments for a “diagnosis unique to transgender patients” yet cover those same treatments for individuals with other medical conditions violate the Equal Protection Clause, and, with regard to the West Virginia plaintiffs, also ACA section 1557 and the Medicaid Act. The court explained that differing medical coverage on the basis of diagnosis (where the diagnosis is as intertwined with the patient’s gender identity as gender dysphoria is) effectively discriminates on the basis of an individual’s gender identity and sex. The court determined the coverage exclusions were facially discriminatory and were not substantially related to an important government interest.
GROOM INSIGHT: The equal protection issues the plaintiffs raised do not apply to private employers because the Fourteenth Amendment only prohibits certain activities by state actors. Non-federal governmental plans, however, assess their plans to determine whether any exclusions related to gender dysphoria expose the plan to potential liability.
Groom insight: of note, in its discussion of the section 1557 claim, the fourth circuit applied bostock and relied on caselaw interpreting title vii to evaluate a claim arising under title ix for purposes of determining whether the west virginia medicaid exclusions violated section 1557. the fourth circuit did not reach the merits of the appellant’s argument that “gender identity” is a distinct concept under title ix from “sex.” but, the court did determine that west virginia’s medicaid policy violates even binary conceptions of sex discrimination ( i.e ., male or female biological differences, and not “gender identity”) under section 1557. the court’s reliance on bostock in evaluating claims of sex discrimination under section 1557 could have repercussions for group health plans sponsored by private and public employers, their third-party administrators, and health insurers because of stronger arguments available to plaintiffs that limitations on gender-affirming care create per se liability for a plan subject to section 1557. .
In the wake of both decisions, plan sponsors, third party administrators, and insurers should consider actively reviewing and updating their policies, perform internal audits to ensure compliance, and train or re-train personnel to reduce potential exposure under Title VII and related non-discrimination laws, such as section 1557. Risks for regulated entities under section 1557 will remain even if the implementing regulations are invalidated by courts or revised under future administrations, as many courts could construe the ACA itself to cover gender-affirming healthcare services. Importantly, neither case addressed any protections available to private employers under a variety of religious freedom laws, which could materially alter the application of these decisions to some private employers and potentially their third-party administrators. Moreover, plan sponsors should assess their benefit designs to ensure that limitations applicable to care related to gender dysphoria do not violate the MHPAEA parity requirements. Plan sponsors can minimize risk by maintaining up-to-date nonquantitative treatment limitations (“NQTL”) analyses and carefully evaluating limitations on care related to gender dysphoria, if appropriate.
[1] See e.g., Neese v. Becerra , 23-10078 (2024) (a challenge brought by Texas doctors against the HHS that argues healthcare providers receiving federal financial assistance may lawfully deny or withhold gender affirming care under section 1557; the outcome of this case is pending before the Fifth Circuit).
[2] Lange v. Houston Cnty., Georgia , 101 F.4th 793, 800 (11th Cir. 2024).
[3] Kadel v. Folwell , 100 F.4th 122 (4th Cir. 2024).
Latest Posts
- This Week From the Hill (June 30 – July 7, 2024)
- Open Season for Regulatory Challenges: Supreme Court Overturns Chevron Deference and Expands Opportunities to Attack Federal Rules
- IRS Guidance on New Exceptions to the Penalty Tax for Early Qualified Plan or IRA Withdrawals
- Latest Update to the Ongoing Challenge to the ACA’s Preventive Services Mandate
See more »
DISCLAIMER: Because of the generality of this update, the information provided herein may not be applicable in all situations and should not be acted upon without specific legal advice based on particular situations.
Refine your interests »
Written by:

PUBLISH YOUR CONTENT ON JD SUPRA NOW
- Increased visibility
- Actionable analytics
- Ongoing guidance
Published In:
Groom law group, chartered on:.

"My best business intelligence, in one easy email…"
OUR STORIES
Asahi group employee’s insights on crafting a responsible drinking culture for a better future.
- # Responsible_drinking # Sustainability

The practice of consuming alcohol is steeped in history, tracing its origins to approximately 4,000 BC, during the era of the world's ancient civilizations. Even after thousands of years, alcohol still serves as a source of joy and enrichment in people's lives, acting as a common facilitator of enjoyable moments and social interactions. However, it's crucial to acknowledge that inappropriate drinking habits can result in a multitude of alcohol-related issues, affecting individuals, families, and the broader society. In order to mitigate these issues, Asahi Group has prioritized responsible drinking and is actively promoting initiatives to reduce inappropriate drinking while introducing new, responsible ways to enjoy alcohol. In the first section of this piece, we shed light on Asahi Group's strides towards fostering a culture of responsible drinking. The second part of the article features an interview* with our employee spearheading these efforts, offering an insightful look into the facets of responsible drinking and the vision for the future of alcohol beverage culture that Asahi Group aspires to cultivate through proper drinking habits. *This interview was conducted in 2023.
Policy Development and Cross-Industry Collaboration toward the Realization of Responsible Drinking
In 2019, Asahi Group set forth the Asahi Group Responsible Drinking Principles. To advance these principles, the company introduced the global slogan “Responsible Drinking Ambassador”in 2020. The inclusion of the word “Ambassador” in the slogan represents the Group’s resolve to influence the behavior of every employee involved in the alcohol beverage business. The Group creates videos and communication tools, and provides training to raise employee awareness about their role as an ambassador and to encourage learning.
The Group is also a member of the International Alliance for Responsible Drinking (IARD), a worldwide non-profit organization. IARD actively promotes responsible drinking initiatives and partners with leading global alcohol beverage manufacturers to maintain industry stability and health. A significant part of IARD's work involves encouraging responsible marketing to prevent underage drinking. In line with this, the Group is committed to abiding by the Digital Guiding Principles, a set of global standards established by IARD to protect minors from exposure to online alcohol advertisements. While all IARD members are working towards compliance with these principles, the Asahi Group has outlined a timeline, aiming to achieve full compliance by 2024.
Responsible Alcohol Use Calls for Understanding and Respecting One’s Limits
Seiya Tanaka, who works in the Sustainability Department at Asahi Group Holdings, takes charge of“responsible drinking” as a key issue. His responsibilities include overseeing global meetings, implementing strategies and policies resolved at meetings, and working on a project aimed at increasing the understanding of intricate alcohol-related issues and providing a comprehensive perspective. We reached out to Mr. Tanaka to get his managerial perspective on appropriate alcohol consumption as well as to understand the significance of Asahi Group’s advocacy for responsible drinking.

――First of all, please tell us about your job.
Tanaka: Part of my responsibility towards responsible drinking includes participating in a project aimed at visualizing the complexities of alcohol-related issues that lead to inappropriate drinking habits. To gain a deeper understanding of these complex structures, we are conducting interviews with a wide range of stakeholders. These include students, educational institutions, restaurants, medical facilities, as well as individuals and families grappling with alcohol-related challenges. The insights we gather from these interviews will be instrumental in the development and implementation of initiatives that aim to address specific alcohol-related issues together with the stakeholders. Furthermore, we intend to conduct workshops that will help visualize the complexities of alcohol-related issues. These workshops will provide a platform for stakeholders to collectively understand these issues better and brainstorm potential solutions.
――What sorts of drinking habits do you and those around you have?
Tanaka: I have opportunities to drink with people of a broad range of ages, and I get the impression that more and more people are drinking at their own pace and within their own limits. On a personal note, I ensure that I drink in line with my physical state and the plans I have for the following day. For instance, I often intersperse my alcohol beverages with non-alcohol drinks. I've noticed that many people now opt solely for non-alcohol beverages. While there are still plenty who enjoy alcohol, it's common to see them reminding each other against excessive drinking. This shift has created a more inclusive environment, where both drinkers and non-drinkers can enjoy social occasions together.
――Do you feel that your thoughts on alcohol have changed over time?
Tanaka: In my earlier days, both as a student and a fresh employee, I used to admire the ability to consume large amounts of alcohol. However, I've come to realize that everyone has a different tolerance for alcohol and a pace at which they feel comfortable drinking. It seems to me that more and more people are respecting each other's drinking preferences and pace, regardless of their alcohol tolerance, and are still able to enjoy each other's company.
――In terms of health and safety, what is important in ensuring proper alcohol consumption?
Tanaka: I think the most important thing is to know your limits and control the pace and volume of your drinking. In recent years, the numbers of non-alcohol and low-alcohol products are on the rise, and even those who enjoy alcohol have a broader range of choices. They can occasionally opt for a non-alcohol drink or one with lower alcohol content, adding variety to their drinking experience.
Pursuing Responsible and Appropriate Drinking through a Multifaceted Approach, of which only an Alcohol Beverage Manufacturer is Capable

What do you see as the significance of Asahi Group, an alcohol beverage manufacturer, promoting appropriate drinking?
Tanaka: Inappropriate drinking and the resultant alcohol-related problems can be, to some extent, prevented or mitigated through proper education and cultivating a healthier attitude towards alcohol beverages. Beyond raising awareness, we are committed to promoting responsible drinking and reducing alcohol-related problems through our business operations. This includes introducing non-alcohol and low-alcohol products, which, as an alcohol beverage manufacturer, we are uniquely positioned to develop. I believe this highlights the importance of the Group's active promotion. I also feel that our role is to create an environment in which people can enjoy at their own pace, by increasing the number of products available to consumers.
――What do you consider a “healthy alcohol beverage culture enjoyable by both drinkers and non-drinkers alike”?
Tanaka: Surely, everyone wants to be able to drink whatever they like at their own pace. While I’m sure that it varies by time period, country, and culture, some people may have experienced the unspoken pressure to “drink as much as everyone else.” In essence, enjoying alcohol boils down to personal freedom, and everyone’s uniqueness should be respected. This includes honoring the choice of those who opt not to drink. I believe that creating an environment in which everyone is able to drink at their own individual pace and according to their preferences will lead to even greater enjoyment. In my view, the foundation of a truly enjoyable life lies in each person's ability to freely make their own choices.
――What sort of relationship between people and alcohol is the responsible drinking project seeking to achieve?
Tanaka: Alcohol-related problems are characterized by a complex interplay of various factors, such as an individual’s traits, society, culture, and values. They are not easy to overcome. However, I believe that if people build relationships in which they can safely enjoy alcohol beverages, with the products and business activities that we, the members of Asahi Group, provide playing a part, we will be able to create a society where everyone can enjoy life in their own way. The tradition of toasting helps build relationships between people, and makes each person’s life more enriched and enjoyable. That is the future we are aiming for.
Profile: Seiya Tanaka Joined Asahi Breweries in 2017. Assigned to the Nagano Branch Office and placed in charge of on-premise sales in the Minami-Shinshu region. Transferred to the Asahi Group Holdings Sustainability Division in 2021. Currently in charge of “responsible drinking” as a key issue, with duties including the promotion of the Group’s strategies and initiative policies, and collaboration with various regional headquarters. (As of 2023)
For more information on Asahi Group’s promotion of responsible drinking, please see the following webpage. Responsible Drinking
Share this story
- Planet Positivity in Action
- Responsibility in our Communities
- Innovating for the Future
- #Environment
- #Communities
- #Innovation
- #Responsible_drinking
- #Sustainability
- Site search
SARS-CoV-2 in animals

Since the initial outbreak of SARS-CoV-2 (the virus that causes COVID-19), there have been numerous reports of animals becoming infected with the virus. Although the outbreak is over, the disease is now endemic in people, meaning the risk remains of animals becoming exposed to the virus.
There’s still a lot to learn about how SARS-CoV-2 affects different animal species, but the primary domestic animals that have been infected are cats and dogs. Other susceptible pets may include ferrets and hamsters.
Several non-domestic animal species have been diagnosed with SARS-CoV-2 infection as well, including these:
- Animals in zoos, sanctuaries, and rehabilitation facilities, particularly big cats like lions, tigers, and snow leopards; gorillas; and otters
- Mink on mink farms
- Wild white-tailed deer and mule deer
See a full breakdown of U.S. animals with confirmed SARS-CoV-2 infection
The good news is there’s no cause to worry. Overall, the chance of people catching the virus from an animal is far less than the chance of us catching it from another person. What’s more, some simple preventive measures can help protect animals from catching SARS-CoV-2 from us.
What are the clinical signs of SARS-CoV-2 in animals?
Some animals with SARS-CoV-2 may have signs of illness, while others may not. For animals with signs, these can include a combination of the following:
- Difficulty breathing/shortness of breath
- Discharge from the nose or eyes
If your animal is having difficulty breathing and/or has some of these other signs, immediately contact your veterinarian, who can advise you on the best action to take. Note that these signs also can be found with other, more common diseases, and your veterinarian likely will explore those other possibilities, too.
How is SARS-CoV-2 spread in animals?
We’re still learning about how SARS-CoV-2 is spread between people and animals. Domestic animals do not get COVID-19 like humans do, but under natural conditions, pet cats—and, to a lesser extent, pet dogs—may become infected with SARS-CoV-2 after close and prolonged contact with an infected person. There is limited evidence that infected cats or dogs spread the virus to other animals, and transmission from pets to people is rare, even with close contact.
When it comes non-domestic species, in most cases infected animal caretakers or farm workers have been the initial source of the virus for animals. On mink farms, once the virus is introduced, it can rapidly spread among the mink as well as to other animals (domestic or wild) on or near the farm. Animal-to-animal transmission also may occur among other animal species that are housed together or close to each other. Transmission from non-domestic species to people is rare.
How is SARS-CoV-2 diagnosed in animals?
Veterinarians may suspect an animal has SARS-CoV-2 based on the signs the animal is showing and a history of known or possible contact with an infected person. Most pets will not need to be tested for SARS-CoV-2.
Unlike in people, there are no in-home tests for SARS-CoV-2 in animals. Rather, in the United States, whether to test any animal for the virus is a formal decision made collaboratively between local, state, or federal public health and animal health officials.
How is SARS-CoV-2 treated in animals?
In the rare chance that your pet is diagnosed with SARS-CoV-2, your veterinarian will work with you to develop a treatment plan. Most cases in pets are mild and resolve with supportive care, such as ample fluids, good nutrition, and rest. Your veterinarian may recommend you isolate your pet at home, depending on the signs the animal is showing.
If your veterinarian does recommend home isolation and you’re able to provide care for the animal:
- Follow your veterinarian’s instructions for care.
- Do not put a mask on your pet.
- Keep your pet at home, except to get veterinary care.
- If your pet is a cat, keep them indoors.
- Protect yourself and others by following the recommendations of the Centers for Disease Control and Prevention (CDC) for preventing transmission of COVID-19.
- Further protect yourself by washing your hands before and after handling your pet, and when handling your pet’s food, waste, litter box, or supplies.
- Keep the pet separated from any people the CDC has identified as being at increased risk from COVID-19, such as those over 65 years old or with chronic lung or heart disease, diabetes, or compromised immune systems.
- Monitor daily how your pet is doing, and if they seem to be getting worse or developing new signs of illness, call your veterinarian.
Also be sure to follow your veterinarian’s advice on when it’s safe to end the home isolation.
How can I protect my animals against SARS-CoV-2?
The best way to protect most animals against SARS-CoV-2 is to reduce the risk of their exposure to the virus through infected people. The only animal vaccine in the United States is a mink coronavirus vaccine that was first conditionally licensed by the USDA during the pandemic.
If you or another person in your household have COVID-19:
- Restrict contact with pets and other animals, just as you would restrict contact with other people.
- Have an unaffected member of your household or business take care of feeding and otherwise caring for any animals, including pets.
- If you have a service animal or you must care for your animals, then wear a mask; don’t share food, kiss, snuggle, hug, or sleep with them; and wash your hands before and after any contact with them.
Note that there is no reason to remove pets from homes, even if someone in your home has COVID-19, unless there is risk that the pet itself will not able to be cared for appropriately.
More resources
- Animals and COVID-19 (CDC)
- What you should know about COVID-19 and pets (CDC)
Additional information for veterinarians
In the United States, the decision to formally test any animal for SARS-CoV-2 is made using a one health approach. Veterinarians who strongly suspect a patient is infected are advised to contact their designated public health and animal health officials within their jurisdiction, such as state public health veterinarians and/or state animal health officials. The USDA's National Veterinary Services Laboratories perform confirmatory testing, and the results are reported online . Confirmed cases are then reported to the World Organisation for Animal Health (WOAH).
For more information on testing, reporting, and managing animals with SARS-CoV-2, check out the USDA's and CDC’s resources on the topics.
United Patients’ Billing Tactic Appeal Fails on Standing Grounds
By Jacklyn Wille

UnitedHealth Group Inc. defeated an appeal challenging its controversial billing practice of reimbursing doctors through debt cancellation because the patients who filed suit hadn’t suffered an injury giving them standing, the Eighth Circuit ruled Monday.
Plaintiffs Rebecca Smith and Cristine Ghanim didn’t allege that United breached a contractual term or otherwise injured them through its conduct, the US Court of Appeals for the Eighth Circuit said, affirming the lower court’s ruling. The billing practice they challenge—known as cross-plan offsetting—is explicitly authorized by the terms of their health plans, the court said.
The patients said they’d been harmed because United’s failure ...
Learn more about Bloomberg Law or Log In to keep reading:
Learn about bloomberg law.
AI-powered legal analytics, workflow tools and premium legal & business news.
Already a subscriber?
Log in to keep reading or access research tools.
Human Subjects Office
Medical terms in lay language.
Please use these descriptions in place of medical jargon in consent documents, recruitment materials and other study documents. Note: These terms are not the only acceptable plain language alternatives for these vocabulary words.
This glossary of terms is derived from a list copyrighted by the University of Kentucky, Office of Research Integrity (1990).
For clinical research-specific definitions, see also the Clinical Research Glossary developed by the Multi-Regional Clinical Trials (MRCT) Center of Brigham and Women’s Hospital and Harvard and the Clinical Data Interchange Standards Consortium (CDISC) .
Alternative Lay Language for Medical Terms for use in Informed Consent Documents
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
ABDOMEN/ABDOMINAL body cavity below diaphragm that contains stomach, intestines, liver and other organs ABSORB take up fluids, take in ACIDOSIS condition when blood contains more acid than normal ACUITY clearness, keenness, esp. of vision and airways ACUTE new, recent, sudden, urgent ADENOPATHY swollen lymph nodes (glands) ADJUVANT helpful, assisting, aiding, supportive ADJUVANT TREATMENT added treatment (usually to a standard treatment) ANTIBIOTIC drug that kills bacteria and other germs ANTIMICROBIAL drug that kills bacteria and other germs ANTIRETROVIRAL drug that works against the growth of certain viruses ADVERSE EFFECT side effect, bad reaction, unwanted response ALLERGIC REACTION rash, hives, swelling, trouble breathing AMBULATE/AMBULATION/AMBULATORY walk, able to walk ANAPHYLAXIS serious, potentially life-threatening allergic reaction ANEMIA decreased red blood cells; low red cell blood count ANESTHETIC a drug or agent used to decrease the feeling of pain, or eliminate the feeling of pain by putting you to sleep ANGINA pain resulting from not enough blood flowing to the heart ANGINA PECTORIS pain resulting from not enough blood flowing to the heart ANOREXIA disorder in which person will not eat; lack of appetite ANTECUBITAL related to the inner side of the forearm ANTIBODY protein made in the body in response to foreign substance ANTICONVULSANT drug used to prevent seizures ANTILIPEMIC a drug that lowers fat levels in the blood ANTITUSSIVE a drug used to relieve coughing ARRHYTHMIA abnormal heartbeat; any change from the normal heartbeat ASPIRATION fluid entering the lungs, such as after vomiting ASSAY lab test ASSESS to learn about, measure, evaluate, look at ASTHMA lung disease associated with tightening of air passages, making breathing difficult ASYMPTOMATIC without symptoms AXILLA armpit
BENIGN not malignant, without serious consequences BID twice a day BINDING/BOUND carried by, to make stick together, transported BIOAVAILABILITY the extent to which a drug or other substance becomes available to the body BLOOD PROFILE series of blood tests BOLUS a large amount given all at once BONE MASS the amount of calcium and other minerals in a given amount of bone BRADYARRHYTHMIAS slow, irregular heartbeats BRADYCARDIA slow heartbeat BRONCHOSPASM breathing distress caused by narrowing of the airways
CARCINOGENIC cancer-causing CARCINOMA type of cancer CARDIAC related to the heart CARDIOVERSION return to normal heartbeat by electric shock CATHETER a tube for withdrawing or giving fluids CATHETER a tube placed near the spinal cord and used for anesthesia (indwelling epidural) during surgery CENTRAL NERVOUS SYSTEM (CNS) brain and spinal cord CEREBRAL TRAUMA damage to the brain CESSATION stopping CHD coronary heart disease CHEMOTHERAPY treatment of disease, usually cancer, by chemical agents CHRONIC continuing for a long time, ongoing CLINICAL pertaining to medical care CLINICAL TRIAL an experiment involving human subjects COMA unconscious state COMPLETE RESPONSE total disappearance of disease CONGENITAL present before birth CONJUNCTIVITIS redness and irritation of the thin membrane that covers the eye CONSOLIDATION PHASE treatment phase intended to make a remission permanent (follows induction phase) CONTROLLED TRIAL research study in which the experimental treatment or procedure is compared to a standard (control) treatment or procedure COOPERATIVE GROUP association of multiple institutions to perform clinical trials CORONARY related to the blood vessels that supply the heart, or to the heart itself CT SCAN (CAT) computerized series of x-rays (computerized tomography) CULTURE test for infection, or for organisms that could cause infection CUMULATIVE added together from the beginning CUTANEOUS relating to the skin CVA stroke (cerebrovascular accident)
DERMATOLOGIC pertaining to the skin DIASTOLIC lower number in a blood pressure reading DISTAL toward the end, away from the center of the body DIURETIC "water pill" or drug that causes increase in urination DOPPLER device using sound waves to diagnose or test DOUBLE BLIND study in which neither investigators nor subjects know what drug or treatment the subject is receiving DYSFUNCTION state of improper function DYSPLASIA abnormal cells
ECHOCARDIOGRAM sound wave test of the heart EDEMA excess fluid collecting in tissue EEG electric brain wave tracing (electroencephalogram) EFFICACY effectiveness ELECTROCARDIOGRAM electrical tracing of the heartbeat (ECG or EKG) ELECTROLYTE IMBALANCE an imbalance of minerals in the blood EMESIS vomiting EMPIRIC based on experience ENDOSCOPIC EXAMINATION viewing an internal part of the body with a lighted tube ENTERAL by way of the intestines EPIDURAL outside the spinal cord ERADICATE get rid of (such as disease) Page 2 of 7 EVALUATED, ASSESSED examined for a medical condition EXPEDITED REVIEW rapid review of a protocol by the IRB Chair without full committee approval, permitted with certain low-risk research studies EXTERNAL outside the body EXTRAVASATE to leak outside of a planned area, such as out of a blood vessel
FDA U.S. Food and Drug Administration, the branch of federal government that approves new drugs FIBROUS having many fibers, such as scar tissue FIBRILLATION irregular beat of the heart or other muscle
GENERAL ANESTHESIA pain prevention by giving drugs to cause loss of consciousness, as during surgery GESTATIONAL pertaining to pregnancy
HEMATOCRIT amount of red blood cells in the blood HEMATOMA a bruise, a black and blue mark HEMODYNAMIC MEASURING blood flow HEMOLYSIS breakdown in red blood cells HEPARIN LOCK needle placed in the arm with blood thinner to keep the blood from clotting HEPATOMA cancer or tumor of the liver HERITABLE DISEASE can be transmitted to one’s offspring, resulting in damage to future children HISTOPATHOLOGIC pertaining to the disease status of body tissues or cells HOLTER MONITOR a portable machine for recording heart beats HYPERCALCEMIA high blood calcium level HYPERKALEMIA high blood potassium level HYPERNATREMIA high blood sodium level HYPERTENSION high blood pressure HYPOCALCEMIA low blood calcium level HYPOKALEMIA low blood potassium level HYPONATREMIA low blood sodium level HYPOTENSION low blood pressure HYPOXEMIA a decrease of oxygen in the blood HYPOXIA a decrease of oxygen reaching body tissues HYSTERECTOMY surgical removal of the uterus, ovaries (female sex glands), or both uterus and ovaries
IATROGENIC caused by a physician or by treatment IDE investigational device exemption, the license to test an unapproved new medical device IDIOPATHIC of unknown cause IMMUNITY defense against, protection from IMMUNOGLOBIN a protein that makes antibodies IMMUNOSUPPRESSIVE drug which works against the body's immune (protective) response, often used in transplantation and diseases caused by immune system malfunction IMMUNOTHERAPY giving of drugs to help the body's immune (protective) system; usually used to destroy cancer cells IMPAIRED FUNCTION abnormal function IMPLANTED placed in the body IND investigational new drug, the license to test an unapproved new drug INDUCTION PHASE beginning phase or stage of a treatment INDURATION hardening INDWELLING remaining in a given location, such as a catheter INFARCT death of tissue due to lack of blood supply INFECTIOUS DISEASE transmitted from one person to the next INFLAMMATION swelling that is generally painful, red, and warm INFUSION slow injection of a substance into the body, usually into the blood by means of a catheter INGESTION eating; taking by mouth INTERFERON drug which acts against viruses; antiviral agent INTERMITTENT occurring (regularly or irregularly) between two time points; repeatedly stopping, then starting again INTERNAL within the body INTERIOR inside of the body INTRAMUSCULAR into the muscle; within the muscle INTRAPERITONEAL into the abdominal cavity INTRATHECAL into the spinal fluid INTRAVENOUS (IV) through the vein INTRAVESICAL in the bladder INTUBATE the placement of a tube into the airway INVASIVE PROCEDURE puncturing, opening, or cutting the skin INVESTIGATIONAL NEW DRUG (IND) a new drug that has not been approved by the FDA INVESTIGATIONAL METHOD a treatment method which has not been proven to be beneficial or has not been accepted as standard care ISCHEMIA decreased oxygen in a tissue (usually because of decreased blood flow)
LAPAROTOMY surgical procedure in which an incision is made in the abdominal wall to enable a doctor to look at the organs inside LESION wound or injury; a diseased patch of skin LETHARGY sleepiness, tiredness LEUKOPENIA low white blood cell count LIPID fat LIPID CONTENT fat content in the blood LIPID PROFILE (PANEL) fat and cholesterol levels in the blood LOCAL ANESTHESIA creation of insensitivity to pain in a small, local area of the body, usually by injection of numbing drugs LOCALIZED restricted to one area, limited to one area LUMEN the cavity of an organ or tube (e.g., blood vessel) LYMPHANGIOGRAPHY an x-ray of the lymph nodes or tissues after injecting dye into lymph vessels (e.g., in feet) LYMPHOCYTE a type of white blood cell important in immunity (protection) against infection LYMPHOMA a cancer of the lymph nodes (or tissues)
MALAISE a vague feeling of bodily discomfort, feeling badly MALFUNCTION condition in which something is not functioning properly MALIGNANCY cancer or other progressively enlarging and spreading tumor, usually fatal if not successfully treated MEDULLABLASTOMA a type of brain tumor MEGALOBLASTOSIS change in red blood cells METABOLIZE process of breaking down substances in the cells to obtain energy METASTASIS spread of cancer cells from one part of the body to another METRONIDAZOLE drug used to treat infections caused by parasites (invading organisms that take up living in the body) or other causes of anaerobic infection (not requiring oxygen to survive) MI myocardial infarction, heart attack MINIMAL slight MINIMIZE reduce as much as possible Page 4 of 7 MONITOR check on; keep track of; watch carefully MOBILITY ease of movement MORBIDITY undesired result or complication MORTALITY death MOTILITY the ability to move MRI magnetic resonance imaging, diagnostic pictures of the inside of the body, created using magnetic rather than x-ray energy MUCOSA, MUCOUS MEMBRANE moist lining of digestive, respiratory, reproductive, and urinary tracts MYALGIA muscle aches MYOCARDIAL pertaining to the heart muscle MYOCARDIAL INFARCTION heart attack
NASOGASTRIC TUBE placed in the nose, reaching to the stomach NCI the National Cancer Institute NECROSIS death of tissue NEOPLASIA/NEOPLASM tumor, may be benign or malignant NEUROBLASTOMA a cancer of nerve tissue NEUROLOGICAL pertaining to the nervous system NEUTROPENIA decrease in the main part of the white blood cells NIH the National Institutes of Health NONINVASIVE not breaking, cutting, or entering the skin NOSOCOMIAL acquired in the hospital
OCCLUSION closing; blockage; obstruction ONCOLOGY the study of tumors or cancer OPHTHALMIC pertaining to the eye OPTIMAL best, most favorable or desirable ORAL ADMINISTRATION by mouth ORTHOPEDIC pertaining to the bones OSTEOPETROSIS rare bone disorder characterized by dense bone OSTEOPOROSIS softening of the bones OVARIES female sex glands
PARENTERAL given by injection PATENCY condition of being open PATHOGENESIS development of a disease or unhealthy condition PERCUTANEOUS through the skin PERIPHERAL not central PER OS (PO) by mouth PHARMACOKINETICS the study of the way the body absorbs, distributes, and gets rid of a drug PHASE I first phase of study of a new drug in humans to determine action, safety, and proper dosing PHASE II second phase of study of a new drug in humans, intended to gather information about safety and effectiveness of the drug for certain uses PHASE III large-scale studies to confirm and expand information on safety and effectiveness of new drug for certain uses, and to study common side effects PHASE IV studies done after the drug is approved by the FDA, especially to compare it to standard care or to try it for new uses PHLEBITIS irritation or inflammation of the vein PLACEBO an inactive substance; a pill/liquid that contains no medicine PLACEBO EFFECT improvement seen with giving subjects a placebo, though it contains no active drug/treatment PLATELETS small particles in the blood that help with clotting POTENTIAL possible POTENTIATE increase or multiply the effect of a drug or toxin (poison) by giving another drug or toxin at the same time (sometimes an unintentional result) POTENTIATOR an agent that helps another agent work better PRENATAL before birth PROPHYLAXIS a drug given to prevent disease or infection PER OS (PO) by mouth PRN as needed PROGNOSIS outlook, probable outcomes PRONE lying on the stomach PROSPECTIVE STUDY following patients forward in time PROSTHESIS artificial part, most often limbs, such as arms or legs PROTOCOL plan of study PROXIMAL closer to the center of the body, away from the end PULMONARY pertaining to the lungs
QD every day; daily QID four times a day
RADIATION THERAPY x-ray or cobalt treatment RANDOM by chance (like the flip of a coin) RANDOMIZATION chance selection RBC red blood cell RECOMBINANT formation of new combinations of genes RECONSTITUTION putting back together the original parts or elements RECUR happen again REFRACTORY not responding to treatment REGENERATION re-growth of a structure or of lost tissue REGIMEN pattern of giving treatment RELAPSE the return of a disease REMISSION disappearance of evidence of cancer or other disease RENAL pertaining to the kidneys REPLICABLE possible to duplicate RESECT remove or cut out surgically RETROSPECTIVE STUDY looking back over past experience
SARCOMA a type of cancer SEDATIVE a drug to calm or make less anxious SEMINOMA a type of testicular cancer (found in the male sex glands) SEQUENTIALLY in a row, in order SOMNOLENCE sleepiness SPIROMETER an instrument to measure the amount of air taken into and exhaled from the lungs STAGING an evaluation of the extent of the disease STANDARD OF CARE a treatment plan that the majority of the medical community would accept as appropriate STENOSIS narrowing of a duct, tube, or one of the blood vessels in the heart STOMATITIS mouth sores, inflammation of the mouth STRATIFY arrange in groups for analysis of results (e.g., stratify by age, sex, etc.) STUPOR stunned state in which it is difficult to get a response or the attention of the subject SUBCLAVIAN under the collarbone SUBCUTANEOUS under the skin SUPINE lying on the back SUPPORTIVE CARE general medical care aimed at symptoms, not intended to improve or cure underlying disease SYMPTOMATIC having symptoms SYNDROME a condition characterized by a set of symptoms SYSTOLIC top number in blood pressure; pressure during active contraction of the heart
TERATOGENIC capable of causing malformations in a fetus (developing baby still inside the mother’s body) TESTES/TESTICLES male sex glands THROMBOSIS clotting THROMBUS blood clot TID three times a day TITRATION a method for deciding on the strength of a drug or solution; gradually increasing the dose T-LYMPHOCYTES type of white blood cells TOPICAL on the surface TOPICAL ANESTHETIC applied to a certain area of the skin and reducing pain only in the area to which applied TOXICITY side effects or undesirable effects of a drug or treatment TRANSDERMAL through the skin TRANSIENTLY temporarily TRAUMA injury; wound TREADMILL walking machine used to test heart function
UPTAKE absorbing and taking in of a substance by living tissue
VALVULOPLASTY plastic repair of a valve, especially a heart valve VARICES enlarged veins VASOSPASM narrowing of the blood vessels VECTOR a carrier that can transmit disease-causing microorganisms (germs and viruses) VENIPUNCTURE needle stick, blood draw, entering the skin with a needle VERTICAL TRANSMISSION spread of disease
WBC white blood cell

IMAGES
VIDEO
COMMENTS
Non-Employees. The theme that should be starting to recur is that only employees can participate in the group health plan on a pre-tax basis. Non-employees cannot pay for their group health insurance coverage through the corporation's Cafeteria Plan nor would they be eligible to participate in an employer's FSA, HRA or HSA. Domestic ...
Group health insurance plans provide numerous tax benefits to both the employer and employee. The money employers pay towards monthly premiums is tax-deductible, and employees' premium payments ...
While a small business with at least one qualified full-time equivalent employee can get group health insurance, a self-employed business owner or sole proprietor with no employees usually would not be eligible for a group health plan. Instead, a sole proprietor could enroll in an individual health insurance plan.
If you opt to offer contract medical insurance, there are four points to keep in mind: 1. Employers can offer the same group plan. As noted above, you can offer contractors the same group plan as your part and full-time employees. You don't have to select a different plan for contractors to access. 2.
A group health plan is most commonly a medical insurance policy an employer offers its employees. The plans are usually the cheapest insurance options if you have access to them. Federal law requires all businesses with 50 or more full-time employees offer a health insurance plan that meets the Affordable Care Act's minimum essential coverage ...
AARP also offers group health insurance. According to AARP, its Essential Premier Health Insurance Plan is similar to the health insurance plans offered by many companies to employees. Membership ...
Group health insurance plans refer to healthcare coverage that is purchased for a group, typically by employers, business owners, or association heads. As opposed to individual health insurance plans that allow anyone to enroll through a marketplace insurance provider, group medical insurance only permits select members or employees of the ...
Thanks for sharing these two options for obtaining group health insurance as a non-employee. It's essential to carefully weigh the costs and benefits of joining associations or exploring small group insurance, depending on individual circumstances and needs. Consulting with an insurance agent is a wise step to make an informed decision about ...
Group Health Insurance Plan: A group health insurance plan is an insurance plan that provides healthcare coverage to a select group of people. Group health insurance plans are one of the major ...
Group health insurance plans refer to the health coverage benefits that apply to a group of members, typically employees of a business or organization. The Social Security Administration (SSA)states that a group health plan (GHP) is based on current employment. Moreover, employers with 20 or more employees must legally offer current workers and ...
Eligibility criteria. Generally, to be eligible for group health insurance, a business must fulfill two main requirements: The business must have at least one qualified full-time or full-time equivalent employee other than the business owner or a spouse. The company must be considered a legal business entity according to its state's regulations.
HLP-ISBA080-GRPHLTH. A "Group Health Plan" (GHP) is health insurance offered by an employer, union or association to its members while they are still working. GHP coverage is based on current employment . Employers with 20 or more employees are required by law to offer current workers and their spouses who are age 65 (or older) the same GHP ...
A group health insurance plan, like a plan purchased through the Small Business Health Options Program (SHOP) or otherwise from a private insurance company, provides coverage to eligible employees. Business owners can offer their employees one plan or a selection of plans to choose from. Small employers (generally those with 1-50 employees) may ...
For one, it is unclear whether a Multiple Employer Welfare Arrangement (MEWA) is created when health or other welfare benefits are provided to non-employee directors. A MEWA is defined as an employee welfare benefit plan providing benefits to the employees of two or more employers (including one or more self-employed individuals). If the board ...
HealthPartners and HealthPartners UnityPoint Health offer group medical insurance and group dental insurance to organizations based in Minnesota, Wisconsin, North Dakota, South Dakota and Iowa. Our national solutions serve members across the country. We also offer retiree group Medicare plans. Our comprehensive, research-based approach to ...
Employer contributions to coverage may also be taxable. Complicating this decision is that some insurance carriers will allow independent contractors to be included in an employer's health plan. But, compliance is the employer's responsibility, not the insurance carrier's. The best answer to whether non-employees can be offered coverage ...
The Takeaway on Group Insurance Eligibility. The bottom line is that group health insurance is typically reserved for regular, full-time employees and their dependents. Any coverage extended to part-time workers or non-traditional dependents is solely at the discretion of the employer. The only requirement is that the employer must provide the ...
The USC-Brookings Schaeffer Initiative for Health Policy recently looked at the data to learn more about this segment of the market. It reported four key findings: 1. Only half of potential ...
They include health savings accounts (HSAs), non-traditional group health plans, medical cost-sharing programs, limited medical (or catastrophic care) plans, and more. Depending on the plan, they can: ... This strategy is an effective recruiting and retention tool because it offers employees a medical insurance plan with tax benefits. The ...
The employer QSEHRA requirements are: Be "small": The business or non-profit must be a "small employer" in the eyes of the IRS, meaning it must have 50 or fewer full-time employees to meet QSEHRA eligibility. Not have a group health plan: The small business or non-profit cannot have a traditional group health plan.
About half of U.S. companies offer health insurance. Among nonprofits with fewer than 50 employers (two-thirds of all nonprofits), 47% offer health insurance benefits to their employees. Sure, health insurance benefits cost money. On average, employers pay $5,179 annually (83 percent of the premium) to cover a single employee and $12,591 ...
An employee may continue health benefits during periods of employer-provided leave as allowed by the insurance plan documents and approved by the health plan insurer. Employers should address in ...
Like a QSEHRA, nonprofits and other businesses can use an ICHRA to reimburse employees tax-free for individual health insurance premiums and other medical expenses. All employers with at least one W-2 employee can offer an ICHRA. This includes businesses, nonprofits, government entities, and religious organizations.
Running a small business involves juggling various responsibilities, from managing finances to ensuring customer satisfaction. One crucial aspect that can significantly impact your business's success is providing health insurance for your employees. Group health insurance offers numerous benefits, making it an essential consideration for small business owners. In this comprehensive blog post ...
Hired coverage means your business has coverage when you or employees drive a rented, leased or borrowed car for business. Non-owned auto applies to employees using their own cars for business. It provides extra coverage over the employee's personal auto coverage for bodily injury and property damage liability. What Is Considered a Hired Auto?
Group health plans, plan sponsors, third party administrators, and health insurance issuers face increasing non-discrimination requirements. In 2024 alone, there have been many notable legal ...
The Group creates videos and communication tools, and provides training to raise employee awareness about their role as an ambassador and to encourage learning. The Group is also a member of the International Alliance for Responsible Drinking (IARD), a worldwide non-profit organization.
Several non-domestic animal species have been diagnosed with SARS-CoV-2 infection as well, including these: Animals in zoos, sanctuaries, and rehabilitation facilities, particularly big cats like lions, tigers, and snow leopards; gorillas; and otters; Mink on mink farms; Wild white-tailed deer and mule deer
UnitedHealth Group Inc. defeated an appeal challenging its controversial billing practice of reimbursing doctors through debt cancellation because the patients who filed suit hadn't suffered an injury giving them standing, the Eighth Circuit ruled Monday. Plaintiffs Rebecca Smith and Cristine Ghanim didn't allege that United breached a contractual term or otherwise injured them through its ...
Human Subjects Office / IRB Hardin Library, Suite 105A 600 Newton Rd Iowa City, IA 52242-1098. Voice: 319-335-6564 Fax: 319-335-7310